Bariatric surgery
Information you need to understand your disease and the tests you may need.
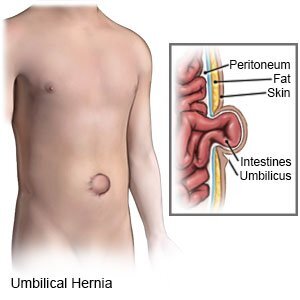
What is sleeve gastrectomy
Sleeve gastrectomy, also called a vertical sleeve gastrectomy, is a surgical weight-loss procedure. This procedure is typically performed laparoscopically, which involves inserting small instruments through multiple small incisions in the upper abdomen.In this operation, surgeons remove part of your stomach and join the remaining portions together to make a new banana-sized stomach or "sleeve." With just a small sack You won't be able to eat as much as you used to, which helps you lose weight. Plus, the surgery removes the part of your stomach that makes a hormone that boosts your appetite.
Why is it done?
Sleeve gastrectomy is done to help you lose excess weight and reduce your risk of potentially life-threatening weight-related health problems, including:
- Heart disease
- High blood pressure
- High cholesterol
- Obstructive sleep apnea
- Type 2 diabetes
- Stroke
- Cancer
- Infertility
Sleeve gastrectomy is typically done only after you've tried to lose weight by improving your diet and exercise habits.
What are the risks associated with it
As with any major surgery, sleeve gastrectomy poses potential health risks, both in the short term and long term.
Risks associated with sleeve gastrectomy can include:
- Excessive bleeding
- Infection
- Adverse reactions to anesthesia
- Blood clots
- Lung or breathing problems
- Leaks from the cut edge of the stomach
- Gastrointestinal obstruction
- Hernias
- Gastroesophageal reflux
- Low blood sugar (hypoglycemia)
- Malnutrition
How it is it done
The surgery takes about an hour. Wel make a few small cuts in your belly and insert a laparoscope -- an instrument with a tiny camera that sends pictures to a monitor. We then insert other medical instruments through the additional cuts and remove 3/4 of your stomach. Finally, we reattach the rest of your stomach to form the "sleeve" or tube.
What to expect from procedure
After sleeve gastrectomy, your diet begins with sugar-free, noncarbonated liquids for the first seven days, then progresses to pureed foods for three weeks, and finally to regular foods approximately four weeks after your surgery. You will be required to take a multivitamin twice a day, a calcium supplement once a day, and a vitamin B-12 injection once a month for life.
You'll have frequent medical checkups to monitor your health in the first several months after weight-loss surgery. You may need laboratory testing, bloodwork and various exams.You may experience changes as your body reacts to the rapid weight loss in the first three to six months after sleeve gastrectomy, including:
- Body aches
- Feeling tired, as if you have the flu
- Feeling cold
- Dry skin
- Hair thinning and hair loss
- Mood changes
Should you opt for the procedure
Sleeve gastrectomy can provide long-term weight loss. The amount of weight you lose depends on your change in lifestyle habits. It is possible to lose approximately 60%, or even more, of your excess weight within two years.
In addition to weight loss, sleeve gastrectomy may improve or resolve conditions related to being overweight, including:
- Heart disease
- High blood pressure
- High cholesterol
- Obstructive sleep apnea
- Type 2 diabetes
- Stroke
- Infertility
Sleeve gastrectomy surgery can also improve your ability to perform routine daily activities, and can help improve your quality of life.
What is Metabolic surgery
Gastric bypass and other weight-loss surgeries — known collectively as bariatric surgery (Metabolic surgery) — involve making changes to your digestive system to help you lose weight. Bariatric surgery is done when diet and exercise haven't worked or when you have serious health problems because of your weight.
Here's a look at common types of bariatric surgery:
- Gastric bypass
- Sleeve gastrectomy
- Biliopancreatic diversion with duodenal switch
Why is it done?
Bariatric surgery is done to help you lose excess weight and reduce your risk of potentially life-threatening weight-related health problems, including:
- Heart disease and stroke
- High blood pressure
- Nonalcoholic fatty liver disease (NAFLD) or nonalcoholic steatohepatitis (NASH)
- Sleep apnea
- Type 2 diabetes
Bariatric surgery is typically done only after you've tried to lose weight by improving your diet and exercise habits.
What are the risks associated with it
Risks associated with the surgical procedure can include:
- Excessive bleeding
- Infection
- Adverse reactions to anesthesia
- Blood clots
- Lung or breathing problems
- Leaks in your gastrointestinal system
- Bowel obstruction
- Dumping syndrome, which leads to diarrhea, flushing, lightheadedness, nausea or vomiting
- Gallstones
- Hernias
- Low blood sugar (hypoglycemia)
- Malnutrition
- Ulcers
- Vomiting
- Acid refluxThe need for a second, or revision, surgery or procedure
- Death (rare)
How it is it done
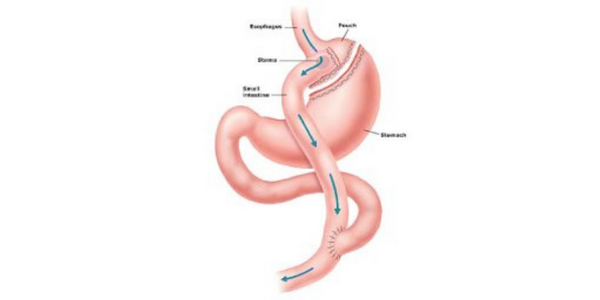
- Gastric bypass. This procedure is the most common method of gastric bypass. It works by decreasing the amount of food you can eat at one sitting and reducing absorption of nutrients. We cut across the top of your stomach, sealing it off from the rest of your stomach. The resulting pouch is about the size of a walnut. Then, we cut the small intestine and sew part of it directly onto the pouch. Food then goes into this small pouch of the stomach and then directly into the small intestine sewn to it.
- Sleeve gastrectomy. With sleeve gastrectomy, about 80% of the stomach is removed, leaving a long, tube-like pouch. This smaller stomach can't hold as much food. It also produces less of the appetite-regulating hormone ghrelin, which may lessen your desire to eat.
- Biliopancreatic diversion with duodenal switch. This is a two-part surgery in which the first step involves performing a procedure similar to a sleeve gastrectomy. The second surgery involves connecting the end portion of the intestine to the duodenum near the stomach bypassing the majority of the intestine.
What to expect from procedure
The specifics of your surgery depend on your individual situation & the type of weight-loss surgery you have. Today, most types of bariatric surgery are performed laparoscopically. Laparoscopic surgery can make your recovery faster and shorter, but it's not suitable for everyone.
Surgery usually takes several hours. Depending on your procedure, you may need to stay a few days in the hospital. After weight-loss surgery, you generally won't be allowed to eat for one to two days so that your stomach and digestive system can heal. Then, you'll follow a specific diet for a few weeks. The diet begins with liquids only, then progresses to pureed, very soft foods, and eventually to regular foods. You may have many restrictions or limits on how much and what you can eat and drink.
You'll also have frequent medical checkups to monitor your health in the first several months after weight-loss surgery. You may need laboratory testing, blood work and various exams.
Should you opt for the procedure
Gastric bypass and other bariatric surgeries can provide long-term weight loss. The amount of weight you lose depends on your type of surgery and your change in lifestyle habits. In addition to weight loss, gastric bypass surgery may improve or resolve conditions often related to being overweight, including:
- Heart disease
- High blood pressure
- Obstructive sleep apnea
- Type 2 diabetes
- Nonalcoholic fatty liver disease (NAFLD) or nonalcoholic steatohepatitis (NASH)
- Gastroesophageal reflux disease (GERD)
- Osteoarthritis (joint pain)
Gastric bypass surgery can also improve your ability to perform routine daily activities, which could help improve your quality of life.
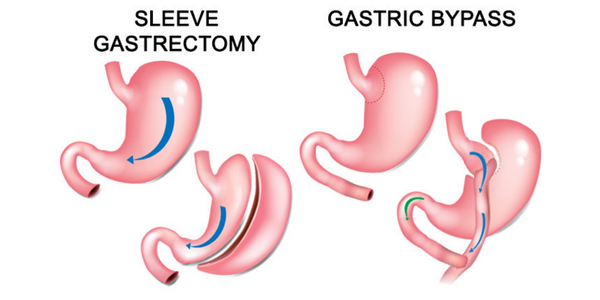
What is gastric balloon
Intragastric balloon placement is a weight-loss procedure that involves placing a saline-filled silicone balloon in your stomach. This helps you lose weight by limiting how much you can eat and making you feel fuller faster.
Why is it done?
The placement of an intragastric balloon helps you lose weight. Weight loss can lower your risk of potentially serious weight-related health problems, such as:
- Gastroesophageal reflux disease (GERD)
- Heart disease or stroke
- High blood pressure
- Obstructive sleep apnea
- Nonalcoholic fatty liver disease (NAFLD) or nonalcoholic steatohepatitis (NASH)
- Type 2 diabetes
Intragastric balloon placement and other weight-loss procedures or surgeries are typically done only after you've tried to lose weight by improving your diet and exercise habits.
What are the risks associated with it
Pain and nausea affect about one-third of people soon after insertion of an intragastric balloon. However, these symptoms usually only last for a few days after balloon placement. These symptoms can usually be managed with oral medications at home.
Although rare, nausea, vomiting and abdominal pain can occur any time after surgery.
A potential risk includes balloon deflation. If the balloon deflates, there's also a risk that it could move through your digestive system. This can cause a blockage that may require an additional procedure or surgery to remove the device.
Other possible risks include overinflation, acute pancreatitis, ulcers or a hole (perforation) in the stomach wall, which might require surgery to fix.
How it is it done
The intragastric balloon procedure is done in the endoscopy unit as an outpatient procedure. You'll be sedated for the procedure.
During the procedure, a thin tube (catheter) loaded with the intragastric balloon will be advanced down your throat into your stomach. Next, an endoscope — a flexible tube with a camera attached will be advanced down your throat into your stomach. The camera will allow visuals to fill the balloon with saline.
The procedure takes about a half-hour. You can normally go home one to two hours after the procedure is finished.
What to expect from procedure
You can have small amounts of clear liquids starting about six hours after the procedure. The liquid diet generally continues until the start of the second week, when you can start eating soft foods. You'll probably be able to start eating regular food around three weeks after the insertion of the intragastric balloon.
Intragastric balloons are left in place for up to 6 months and are then removed using an endoscope to be replaced with a new balloon.
Should you opt for the procedure
An intragastric balloon can make you feel more full faster than you normally would when eating, which often means you'll eat less. The amount of weight you lose also depends on how much you can change your lifestyle habits including diet and exercise.
As with other procedures and surgeries that lead to significant weight loss, the intragastric balloon may help improve or resolve conditions often related to being overweight, including:
- Gastroesophageal reflux disease
- Heart disease
- High blood pressure
- Obstructive sleep apnea
- Osteoarthritis (joint pain)
- Type 2 diabetes
- High cholesterol
- Nonalcoholic fatty liver disease (NAFLD) or nonalcoholic steatohepatitis (NASH)
What is mini gastric bypass
Intragastric balloon placement is a weight-loss procedure that involves placing a saline-filled silicone balloon in your stomach. This helps you lose weight by limiting how much you can eat and making you feel fuller faster.
Why is it done?
The placement of an intragastric balloon helps you lose weight. Weight loss can lower your risk of potentially serious weight-related health problems, such as:
- Gastroesophageal reflux disease (GERD)
- Heart disease or stroke
- High blood pressure
- Obstructive sleep apnea
- Nonalcoholic fatty liver disease (NAFLD) or nonalcoholic steatohepatitis (NASH)
- Type 2 diabetes
Intragastric balloon placement and other weight-loss procedures or surgeries are typically done only after you've tried to lose weight by improving your diet and exercise habits.
What are the risks associated with it
Pain and nausea affect about one-third of people soon after insertion of an intragastric balloon. However, these symptoms usually only last for a few days after balloon placement. These symptoms can usually be managed with oral medications at home.
Although rare, nausea, vomiting and abdominal pain can occur any time after surgery.
A potential risk includes balloon deflation. If the balloon deflates, there's also a risk that it could move through your digestive system. This can cause a blockage that may require an additional procedure or surgery to remove the device.
Other possible risks include overinflation, acute pancreatitis, ulcers or a hole (perforation) in the stomach wall, which might require surgery to fix.
How it is it done
This procedure is the most common method of gastric bypass. It works by decreasing the amount of food you can eat at one sitting and reducing absorption of nutrients. We cut across the top of your stomach, sealing it off from the rest of your stomach. The resulting pouch is about the size of a walnut. Then, we cut the small intestine and sew part of it directly onto the pouch. Food then goes into this small pouch of the stomach and then directly into the small intestine sewn to it.
What to expect from procedure
You can have small amounts of clear liquids starting about six hours after the procedure. The liquid diet generally continues until the start of the second week, when you can start eating soft foods. You'll probably be able to start eating regular food around three weeks after the insertion of the intragastric balloon.
Intragastric balloons are left in place for up to 6 months and are then removed using an endoscope to be replaced with a new balloon.
Should you opt for the procedure
An intragastric balloon can make you feel more full faster than you normally would when eating, which often means you'll eat less. The amount of weight you lose also depends on how much you can change your lifestyle habits including diet and exercise.
As with other procedures and surgeries that lead to significant weight loss, the intragastric balloon may help improve or resolve conditions often related to being overweight, including:
- Gastroesophageal reflux disease
- Heart disease
- High blood pressure
- Obstructive sleep apnea
- Osteoarthritis (joint pain)
- Type 2 diabetes
- High cholesterol
- Nonalcoholic fatty liver disease (NAFLD) or nonalcoholic steatohepatitis (NASH)