Esophagus
Information you need to understand your disease and the tests you may need.
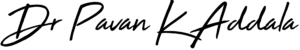
What is GERD reflux
Gastroesophageal reflux disease (GERD) occurs when stomach acid frequently flows back into the tube connecting your mouth and stomach (esophagus). This backwash (acid reflux) can irritate the lining of your esophagus. Most people can manage the discomfort of GERD with lifestyle changes and over-the-counter medications. But some people with GERD may need stronger medications or surgery to ease symptoms.
Causes
Gastroesophageal reflux is when what’s in your stomach backs up into your esophagus. In normal digestion, your LES (A ring of muscle between esophagus and stomach) opens to allow food into your stomach. Then it closes to stop food and acidic stomach juices from flowing back into your esophagus.
Gastroesophageal reflux happens when the LES is weak or relaxes when it shouldn’t. This lets the stomach’s contents flow up into the esophagus. Most people can manage the discomfort of GERD with lifestyle changes and over-the-counter medications. But some people with GERD may need stronger medications or surgery to ease symptoms.
Symptoms
Common signs and symptoms of GERD include:
- A burning sensation in your chest (heartburn), usually after eating, which might be worse at night
- Chest pain
- Difficulty swallowing
- Regurgitation of food or sour liquid
- Sensation of a lump in your throat
- Chronic cough
- Laryngitis
- New or worsening asthma
- Disrupted sleep
GERD/ LPR can occur during the day or night. Patients with LPR often do not experience heartburn and may present with hyperactive bronchi or asthma. Some patients even suffer with frequent sinusitis (infection in air chambers of the facial bones).
Treatment
Reflux can be treated through dietary and lifestyle modifications, medications—usually proton pump inhibitors (PPIs), and in some cases surgery. Certain foods are more likely to cause acid reflux. By removing or limiting these foods from your diet, you can reduce incidences of acid reflux.
You can see symptomatic relief in a few hours to days depending on how severe your problem is and how you adapt your lifestyle in a healthy way. It can take 4-6 weeks for acid burns in the esophagus and larynx to heal, so do not stop medication or dietary/lifestyle modifications without consulting your doctor. It can take 3-4 months for full resolution.
What problems can acid reflux cause?
Long-term reflux can cause laryngeal ulcers or granulomas, vocal fold scarring, pneumonia, lung scarring (interstitial lung disease), Barrett’s esophagus (precancerous), and in some cases esophageal or throat cancer.
Role of surgery in GERD?
Patients with early, on and off reflux symptoms respond well to medications. When damage to E-G junction becomes permanent due to long standing disease, or the patient has the LPR component of reflux disease, surgery is a one point solution for many.
Laparoscopic fundoplication is an advanced laparoscopic surgical technique which is a mechanical correction of the mechanical problem at E-G junction. This is the only near physiological correction which is time tested and accepted around the world. Although there are many endoscopic methods that are coming up from time to time claiming at par results to lap fundoplication, none have the physiologic advantage of lap fundoplication.
Tests to identify GERD/LPR diseases
All patients with suspected reflux disease have to undergo upper GI endoscopy as an initial test for diagnosis and assess complications secondary to prolonged reflux disease. There are a couple of tests which can, not only identify but quantify symptom correlation to reflux. 24 hour ambulatory pH and impedance study and High Resolution Manometry (HRM) objectively identify patients who can benefit from surgery. They also help in ruling out patients with residual symptoms due to reflux after anti reflux surgery. Patients with LPR might need a bronchoscopy to know the extent of damage caused by reflux.
Preventive measures
With good lifestyle adaptation and following dietary modifications as suggested by the surgeon/ dietician it is very unlikely to have a recurrence following surgery. Suggested lifestyle modifications are:
- Do not lie down or exercise directly after eating
- Eat 3-4 small meals a day instead of 2-3 large ones.
- Do not eat anything 2-3 hours before going to bed.
- If reflux is occurring at night, elevate the head of your bed 4-6 inches by putting phone books under the front legs or by buying a wedge pillow.
- Using 2 or more regular pillows can make reflux worse as it causes the body to curl.
- Do not have water or beverages during or immediately after the meal except for a few sips to clear the throat. 15-30 min gap after meal improves digestion and decreases congestion in stomach, resulting in less reflux.
- Do not eat food in a hurry. You tend to gulp some air along with food causing your stomach to bloat. This stretches the E-G sphincter increasing reflux episodes.
- It is preferable to lie on the left side while sleeping as it decreases the pressure on the E-G sphincter and also allows better digestion of the residual food.
- Do not wear clothing that is tight around the waist.
- If you are overweight, try to lose weight.
- Tobacco can cause reflux, so reducing or stopping smoking can be helpful
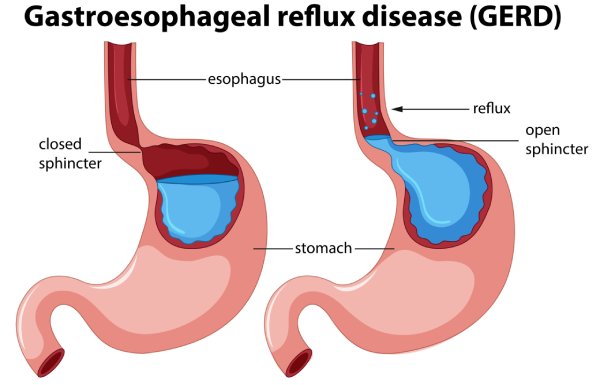
What is Achalasia Cardia
Achalasia cardia is a condition where the sphincter at the lower end of your food pipe (esophagus) fails to relax on swallowing the food. This sphincter called, Lower Esophageal spinster (LES), lies at the junction between esophagus and stomach, channelling food in one way direction - oral to anal end.
Causes
There is no scientific explanation why achalasia happens. But there is some evidence that there is incoordination between the nerves supplying the LES and the muscles of LES due to neurotransmitter (Chemicals secreted by nerves) imbalance.
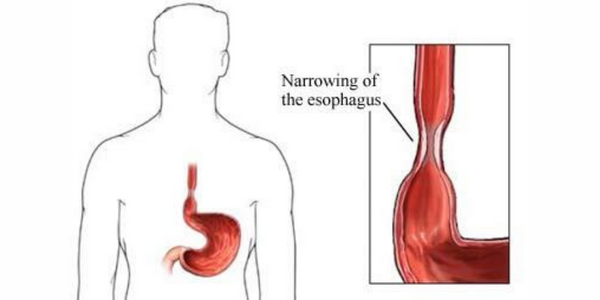
This results in a tight LES, causing difficulty in swallowing. In long standing achalasia, the esophagus above the LES tends to dilate as the muscle hypertrophies and enlarges. Eventually, the esophagus fails to contract, which is important for food to move in forward direction.
Symptoms
Patients with achalasia cardia usually present with difficulty in swallowing, vomiting, halitosis, discomfort in chest, regurgitation of food through nose, choking and cough on lying down, recurrent respiratory infections, sinusitis etc.
Treatment
Since the cause is not known, all treatment options are aimed at relieving the disease and not at curing the disease. Multiple treatment modalities are available for achalasia cardia - medical, endoscopic and surgical myotomy. Medical treatment: Nitrates or Calcium Channel blockers (CCB) are given on a daily basis to relax the LES. Nitrates and CCBs have side effects and have to be used under supervision of a doctor.
Endoscopic methods include: Botox injections at the LES, loosens the sphincter temporarily decreasing symptoms. This method is offered in fragile patients not fit for anesthesia. It has the least success rate. Balloon dilatation is another endoscopic method, wherein the LES muscles are torn by gradually dilating the sphincter muscles using specially designed balloons. Recurrence rates are higher than surgery and less than other less invasive methods. Per Oral Endoscopic Myotomy (POEM), is the new kid in the block for treating achalasia cardia. Introduced in 2015 in India, this method rose to fame in a short time. This procedure is performed under general anesthesia without any visible cuts on the body and has the added advantage of early mobility and discharge after the procedure. Highly technically demanding procedure.
Surgical methods: Surgery can be done by either open method (by giving a large cut in the upper abdomen) or by laparoscopy (keyHole surgery). Whatever the method, the principle is the same - cut open the tight sphincter, expose the EG junction mucosa and cover it with part of the stomach. This is the gold standard against which all other procedures are compared and has got the highest success rates, exceeding 85%
What if achalasia is not treated
Patients tend to lose weight and become malnourished as the food doesn’t reach intestines adequately to be utilized. Patients with long standing achalasia cardia tend to develop atonic esophagus i.e., non functional esophagus which dilates over time resulting in something called a sigmoid esophagus. Patients with sigmoid esophagus need to undergo esophagectomy often as other surgical interventions fail to give good relief of symptoms. Some patients even develop cancer in the esophagus due to constant irritation by the stagnant food material.
Preventive measures
All treatment methods have a tendency to result in acid reflux or chest pain following the procedure. These can decrease by adding anti reflux procedures during surgery, which can not be done with endoscopic methods. Another complication with intervention is perforation of lower esophagus at the time of procedure.
Perforation following endoscopy needs surgical closure, and that occurred during surgery is closed immediately when identified on table. Small perforation missed during surgery can be taken care with endoscopic stunting or redo surgery. Recurrence following a successful myotomy - endoscopically or surgically still occurs. As of now there are no definite criteria to identify the patients in whom achalasia might recur.
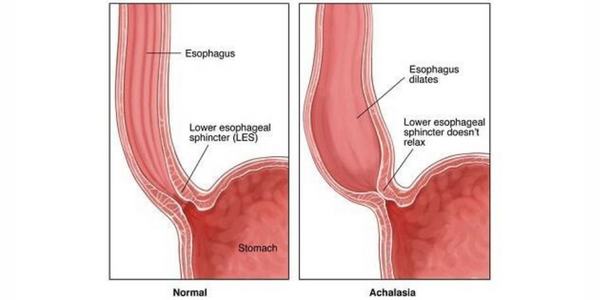
What is Esophageal cancer
Esophageal cancer occurs when cancer cells develop in the esophagus, a tube-like structure that runs from your throat to your stomach. Food goes from the mouth to the stomach through the esophagus. The cancer starts at the inner layer of the esophagus and can spread throughout the other layers of the esophagus and to other parts of the body (metastasis).
Causes
It's not exactly clear what causes esophageal cancer. Esophageal cancer occurs when cells in the esophagus develop changes (mutations) in their DNA. The changes make cells grow and divide out of control. The accumulating abnormal cells form a tumor in the esophagus that can grow to invade nearby structures and spread to other parts of the body.
Factors that cause irritation in the cells of your esophagus and increase your risk of esophageal cancer include:
- Having gastroesophageal reflux disease (GERD)
- Smoking
- Having precancerous changes in the cells of the esophagus (Barrett's esophagus)
- Being obese
- Drinking alcohol
- Having bile reflux
- Having difficulty swallowing because of an esophageal sphincter that won't relax (achalasia)
- Having a steady habit of drinking very hot liquids
- Not eating enough fruits and vegetables
- Undergoing radiation treatment to the chest or upper abdomen
Symptoms
Signs and symptoms of esophageal cancer include:
- Difficulty swallowing (dysphagia)
- Weight loss without trying
- Chest pain, pressure or burning
- Worsening indigestion or heartburn
- Coughing or hoarseness
Early esophageal cancer typically causes no signs or symptoms.
Treatment
To diagnose esophageal cancer, your doctor will review your symptoms, medical history, and examine you. In addition, they may order certain blood tests and X-rays. Tests for esophageal cancer may include:
- Barium swallows X-ray, in which you drink a liquid that coats your esophagus. This makes the esophagus stand out on the X-ray so that your doctor can identify certain problems.
- Endoscopy: the doctor passes an endoscope, a thin, lighted tube, down your throat into your esophagus to examine it. Endoscopic ultrasound uses sound waves to provide more information about the extent of tumor involvement in nearby tissues.
- Biopsy: during an endoscopy, the doctor can take cells or tissue from your esophagus. The cells are examined under a microscope for the presence of cancer.
Other tests, including computed tomography (CT) scans, positron emission tomography (PET) scan, thoracoscopy, and laparoscopy, may be performed to determine if the cancer has spread, or metastasized, outside of the esophagus. This process is called "staging." The doctor needs this information in order to plan your treatment.
Treatment of esophageal cancer depends on many factors, including the stage of the cancer and the overall health of the patient.
- Surgery. Part or all of the esophagus may be removed.
- Radiation therapy. Kills cancer cells with radiation.
- Chemotherapy. Powerful drugs that attack cancer cells throughout the body; typically used in combination with radiation therapy and/or surgery.
- Targeted therapy. Newer treatments that target specific aspects of a cancer to curb cancer growth and spread.
- Immunotherapy. Helps the immune system to attack cancer cells.
- Photodynamic therapy. Targets cancer cells with a special laser light.
- Electrocoagulation. Uses electric current to destroy cancer cells.
- Cryotherapy. Freezes cancer cells to help shrink a tumor.
Endoscopic mucosal resection may be done to treat precancers or very small early cancers by removing the inner lining of the esophagus. Radiofrequency ablation treatment using a device that targets cancer cells with radiofrequency energy is sometimes used for early cancers.
Preventive measures
You can take steps to reduce your risk of esophageal cancer. For instance:
- Quit smoking. If you smoke, talk to your doctor about strategies for quitting. Medications and counseling are available to help you quit. If you don't use tobacco, don't start.
- Drink alcohol in moderation, if at all. If you choose to drink alcohol, do so in moderation. For healthy adults, that means up to one drink a day for women and up to two drinks a day for men.
- Eat more fruits and vegetables. Add a variety of colorful fruits and vegetables to your diet.
- Maintain a healthy weight. If you are overweight or obese, talk to your doctor about strategies to help you lose weight. Aim for a slow and steady weight loss of 1 or 2 pounds a week.
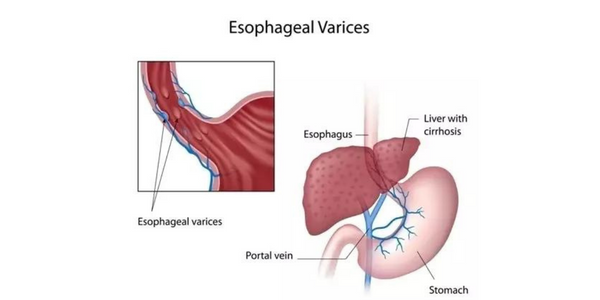
What is Esophageal varices
Esophageal varices are abnormal, enlarged veins in the tube that connects the throat and stomach (esophagus). This condition occurs most often in people with serious liver diseases.
Esophageal varices develop when normal blood flow to the liver is blocked by a clot or scar tissue in the liver. To go around the blockages, blood flows into smaller blood vessels that aren't designed to carry large volumes of blood. The vessels can leak blood or even rupture, causing life-threatening bleeding.
Causes
Esophageal varices sometimes form when blood flow to your liver is blocked, most often by scar tissue in the liver caused by liver disease. The blood flow begins to back up, increasing pressure within the large vein (portal vein) that carries blood to your liver.
This increased pressure (portal hypertension) forces the blood to seek other pathways through smaller veins, such as those in the lowest part of the esophagus. These thin-walled veins balloon with the added blood. Sometimes the veins rupture and bleed.
Causes of esophageal varices include:
- Severe liver scarring (cirrhosis). A number of liver diseases — including hepatitis infection, alcoholic liver disease, fatty liver disease and a bile duct disorder called primary biliary cirrhosis — can result in cirrhosis.
- Blood clot (thrombosis). A blood clot in the portal vein or in a vein that feeds into the portal vein (splenic vein) can cause esophageal varices.
- Parasitic infection. Schistosomiasis is a parasitic infection found in parts of Africa, South America, the Caribbean, the Middle East and East Asia. The parasite can damage the liver, as well as the lungs, intestine, bladder and other organs.
Esophageal varices are more likely to bleed if you have:
- High portal vein pressure. The risk of bleeding increases as the pressure in the portal vein increases (portal hypertension).
- Large varices. The larger the esophageal varices, the more likely they are to bleed.
- Red marks on the varices. When viewed through a thin, flexible tube (endoscope) passed down your throat, some esophageal varices show long, red streaks or red spots. These marks indicate a high risk of bleeding.
- Severe cirrhosis or liver failure. Most often, the more severe your liver disease, the more likely esophageal varices are to bleed.
- Continued alcohol use. Your risk of variceal bleeding is far greater if you continue to drink than if you stop, especially if your disease is alcohol related.
Symptoms
Esophageal varices usually don't cause signs and symptoms unless they bleed. Signs and symptoms of bleeding esophageal varices include:
- Vomiting large amounts of blood
- Black, tarry or bloody stools
- Lightheadedness
- Loss of consciousness in severe cases
Your doctor might suspect esophageal varices if you have signs of liver disease, including:
- Yellow coloration of your skin and eyes (jaundice)
- Easy bleeding or bruising
- Fluid buildup in your abdomen (ascites)
Treatment
In severe cases, a person may need to be placed temporarily on a breathing machine to prevent the lungs from filling with blood. Antibiotics are also given immediately to reduce the risk of sepsis, a life-threatening blood infection.
Aside from the urgent need to stop the bleeding, treatment is also aimed at preventing more bleeding. Procedures that help treat bleeding varices include:
- Banding. A gastroenterologist places small rubber bands directly over the varices. This will stop the bleeding and get rid of the varices.
- Sclerotherapy. A gastroenterologist directly injects the varices with a blood-clotting solution instead of banding them.
- Transjugular Intrahepatic Portosystemic Shunt (TIPS). A radiological procedure in which a stent (a tubular device) is placed in the middle of the liver. The stent connects the hepatic vein with the portal vein. This procedure is done by placing a catheter through a vein in the neck. It is done to relieve the high blood pressure that has built up in the portal vein and the liver.
- Distal Splenorenal Shunt (DSRS). A surgical procedure that connects the splenic vein to the left kidney vein in order to reduce pressure in the varices and control bleeding.
- Liver transplant. A liver transplant may be done in cases of end-stage liver disease.
- Devascularization. A surgical procedure that removes the bleeding varices. This procedure is done when a TIPS or a surgical shunt isn't possible or unsuccessful in controlling the bleeding.
- Esophageal transection. A surgical procedure in which the esophagus is cut through and then stapled back together after the varicies have been tied off. Sometimes there is bleeding at the staple line
Other tests, including computed tomography (CT) scans, positron emission tomography (PET) scan, thoracoscopy, and laparoscopy, may be performed to determine if the cancer has spread, or metastasized, outside of the esophagus. This process is called "staging." The doctor needs this information in order to plan your treatment.
Treatment of esophageal cancer depends on many factors, including the stage of the cancer and the overall health of the patient.
- Surgery. Part or all of the esophagus may be removed.
- Radiation therapy. Kills cancer cells with radiation.
- Chemotherapy. Powerful drugs that attack cancer cells throughout the body; typically used in combination with radiation therapy and/or surgery.
- Targeted therapy. Newer treatments that target specific aspects of a cancer to curb cancer growth and spread.
- Immunotherapy. Helps the immune system to attack cancer cells.
- Photodynamic therapy. Targets cancer cells with a special laser light.
- Electrocoagulation. Uses electric current to destroy cancer cells.
- Cryotherapy. Freezes cancer cells to help shrink a tumor.
Endoscopic mucosal resection may be done to treat precancers or very small early cancers by removing the inner lining of the esophagus. Radiofrequency ablation treatment using a device that targets cancer cells with radiofrequency energy is sometimes used for early cancers.
Preventive measures
Treating the underlying cause of bleeding varices can help prevent their return. Earlier treatment of liver disease may prevent them from developing. Certain medications, including the class of heart drugs called "beta-blockers," may reduce elevated portal pressure and lower the likelihood of bleeding. Long-acting nitroglycerines are also used for this purpose.
What is Dysphagia
Dysphagia is difficulty swallowing — taking more time and effort to move food or liquid from your mouth to your stomach. Dysphagia can be painful. In some cases, swallowing is impossible.Occasional difficulty swallowing, such as when you eat too fast or don't chew your food well enough, usually isn't cause for concern. But persistent dysphagia can be a serious medical condition requiring treatment
A wide range of diseases can cause swallowing problems, which your doctor may call "dysphagia." These include:
- Disturbances of the brain such as those caused by Parkinson's disease, multiple sclerosis, or ALS (amyotrophic lateral sclerosis, or Lou Gehrig's disease)
- Oral or pharynx muscle dysfunction such as from a stroke
- Esophageal narrowing such as from acid reflux or tumors
- Disturbances of the brain such as those caused by Parkinson's disease, multiple sclerosis, or ALS (amyotrophic lateral sclerosis, or Lou Gehrig's disease)
- Oral or pharynx muscle dysfunction such as from a stroke
- Loss of sphincter muscle relaxation (termed "achalasia")
Causes
Any condition that weakens or damages the muscles and nerves used for swallowing or leads to a narrowing of the back of the throat or esophagus can cause dysphagia.
Esophageal dysphagia:
It refers to the sensation of food sticking or getting caught in the base of your throat or in your chest after you've started to swallow. Some of the causes of esophageal dysphagia include:
- Achalasia. When the lower esophageal muscle (sphincter) doesn't relax properly to let food enter the stomach, it can cause food to come back up into the throat.
- Diffuse spasm. This condition causes high-pressure, poorly coordinated contractions of the esophagus, usually after swallowing.
- Esophageal stricture. A narrowed esophagus (stricture) can trap large pieces of food. Tumors or scar tissue, often caused by gastroesophageal reflux disease (GERD), can cause narrowing.
- Esophageal tumors. Difficulty swallowing tends to get progressively worse when esophageal tumors are present due to narrowing of the esophagus.
- Foreign bodies. Sometimes food or another object can partially block the throat or esophagus.
- Esophageal ring. A thin area of narrowing in the lower esophagus can cause difficulty swallowing solid foods off and on.
- GERD. Damage to esophageal tissues from stomach acid backing up into the esophagus can lead to spasm or scarring and narrowing of the lower esophagus.
- Eosinophilic esophagitis. This condition, which might be related to a food allergy, is caused by too many cells called eosinophils in the esophagus.
- Scleroderma. Development of scar-like tissue, causing stiffening and hardening of tissues, can weaken the lower esophageal sphincter.
- Radiation therapy. This cancer treatment can lead to inflammation and scarring of the esophagus.
- Oropharyngeal dysphagia: Certain conditions can weaken the throat muscles, making it difficult to move food from your mouth into your throat and esophagus when you start to swallow.
Causes of oropharyngeal dysphagia include
- High portal vein pressure. Certain disorders — such as multiple sclerosis, muscular dystrophy and Parkinson's disease — can cause dysphagia.
- Neurological damage Sudden neurological damage, such as from a stroke or brain or spinal cord injury, can affect the ability to swallow.
- Pharyngoesophageal diverticulum (Zenker's diverticulum) A small pouch that forms and collects food particles in the throat, often just above the esophagus, leads to difficulty swallowing, gurgling sounds, bad breath, and repeated throat clearing or coughing.
- Cancer Certain cancers and some cancer treatments, such as radiation, can cause difficulty swallowing.
Symptoms
Signs and symptoms associated with dysphagia can include:
- Pain while swallowing
- Inability to swallow
- A sensation of food getting stuck in the throat or chest or behind the breastbone (sternum)
- Drooling
- Food coming back up (regurgitation)
- Hoarseness
- Frequent heartburn
- Food or stomach acid backing up into the throat
- Weight loss
- Coughing or gagging when swallowing
Treatment
Following test can be done to identify & diagnose dysphagia
- Cineradiography: An imaging test in which a camera is used to film internal body structures. During the test, you will be asked to swallow a barium preparation (liquid or other form that lights up under X-ray). An X-ray machine with videotaping capability will be used to view the barium preparations movement through the esophagus. This is often performed under the guidance of a speech pathologist, an expert in swallowing as well as speech.
- Upper endoscopy: A flexible, narrow tube (endoscope) is passed into the esophagus and projects images of the inside of the pharynx and esophagus on a screen for evaluation.
- Manometry: This test measures the timing and strength of esophageal contractions and muscular valve relaxation.
- Impedance and pH test: This test can determine if acid reflux is causing a swallowing problem.
Treatment approaches for esophageal dysphagia might include:
- Surgery : For an esophageal tumor, achalasia or pharyngoesophageal diverticulum, you might need surgery to clear your esophageal path. The type of surgical treatment depends on the cause of dysphagia. Some examples are:
- Laparoscopic Heller myotomy. This involves cutting the muscle at the lower end of the esophagus (sphincter) when it fails to open and release food into the stomach in people who have achalasia.
- Peroral endoscopic myotomy (POEM). The surgeon or gastroenterologist uses an endoscope inserted through the mouth and down the throat to create an incision in the inside lining of the esophagus to treat achalasia Then, as in a Heller myotomy, the surgeon or gastroenterologist cuts the muscle at the lower end of the esophageal sphincter.
- Esophageal dilation. The health care provider inserts a lighted tube (endoscope) into the esophagus and inflates an attached balloon to stretch it (dilation).
- Stent placement. The health care provider can also insert a metal or plastic tube (stent) to prop open a narrowing or blocked esophagus. Some stents are permanent, such as those for people with esophageal cancer, while others are removed later.
- Medications Difficulty swallowing associated with GERD can be treated with prescription oral medications to reduce stomach acid. You might need to take these medications for a long time.
- Diet Your health care provider might prescribe a special diet to help with your symptoms, depending on the cause of the dysphagia.
Preventive measures
- Changing your eating habits. eating smaller, more frequent meals. Cut your food into smaller pieces, chew food thoroughly and eat more slowly. If you have difficulty swallowing liquids, there are products you can buy to thicken liquids.
- Try foods with different textures to see if some cause you more trouble. Thin liquids, such as coffee and juice, are a problem for some people, and sticky foods, such as peanut butter or caramel, can make swallowing difficult. Avoid foods that cause you trouble.
- Limiting alcohol and caffeine. These can dry your mouth and throat, making swallowing more difficult.