Liver
Information you need to understand your disease and the tests you may need.
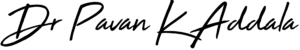
What is liver cirrhosis
Cirrhosis is a late stage of scarring (fibrosis) of the liver caused by many forms of liver diseases and conditions, such as hepatitis and chronic alcoholism.
Each time your liver is injured — whether by disease, excessive alcohol consumption or another cause — it tries to repair itself. In the process, scar tissue forms. As cirrhosis progresses, more and more scar tissue forms, making it difficult for the liver to function (decompensated cirrhosis). Advanced cirrhosis is life-threatening.
Causes
It's important to know the cause of your cirrhosis so you can get the right treatment and keep it from getting worse. The most common causes are:
- Alcohol abuse
- Nonalcoholic fatty liver disease.Obesity raises your chances of this condition
- Hepatitis B or hepatitis C
- Cystic fibrosis
- Diseases that make it hard for your body to process sugars
- Too much iron buildup in your body
- Wilson's disease, where too much copper is stored in the liver
- Autoimmune diseases that cause your body to attack liver cells
- Blockage of the bile duct, which carries digestive enzymes from your liver into the intestines
- Certain genetic digestive disorders
- Some infections, including syphilis and brucellosis
- Bad reactions to certain medications
Symptoms
When signs and symptoms do occur, they may include:
- Fatigue
- Easily bleeding or bruising
- Loss of appetite
- Nausea
- Swelling in your legs, feet or ankles (edema)
- Weight loss
- Itchy skin
- Yellow discoloration in the skin and eyes (jaundice)
- Fluid accumulation in your abdomen (ascites)
- Spiderlike blood vessels on your skin
- Redness in the palms of the hands
- For women, absent or loss of periods not related to menopause
- For men, loss of sex drive, breast enlargement (gynecomastia) or testicular atrophy
- Confusion, drowsiness and slurred speech (hepatic encephalopathy)
Treatment
Often, cirrhosis is first detected through a routine blood test or checkup.
- Laboratory tests. Blood tests to check for signs of liver malfunction, such as excess bilirubin, as well as for certain enzymes that may indicate liver damage. To assess kidney function, your blood is checked for creatinine. You'll be screened for the hepatitis viruses. Your international normalized ratio (INR) is also checked for your blood's ability to clot.
- Imaging tests. Magnetic resonance elastography (MRE) may be recommended. This noninvasive advanced imaging test detects hardening or stiffening of the liver. Other imaging tests, such as MRI, CT and ultrasound, may also be done.
- Biopsy. A tissue sample (biopsy) is not necessarily needed for diagnosis. However, your doctor may use it to identify the severity, extent and cause of liver damage.
Treatment for cirrhosis depends on the cause and extent of your liver damage. The goals of treatment are to slow the progression of scar tissue in the liver and to prevent or treat symptoms and complications of cirrhosis Treatment for the underlying cause of cirrhosis
In early cirrhosis, it may be possible to minimize damage to the liver by treating the underlying cause. The options include:
- Treatment for alcohol dependency
- Weight loss
- Medications to control hepatitis
- Medications to control other causes and symptoms of cirrhosis
- Other medications can relieve certain symptoms, such as itching, fatigue and pain. Nutritional supplements may be prescribed to counter malnutrition associated with cirrhosis and to prevent weak bones (osteoporosis).
Treatment for complications of cirrhosis
- A low-sodium diet and medication to prevent fluid buildup in the body may help control ascites and swelling.
- Portal hypertension. Certain blood pressure medications may control increased pressure in the veins that supply the liver (portal hypertension) and prevent severe bleeding.
- Infections. You may receive antibiotics or other treatments for infections.
- Periodic blood tests and ultrasound exams to look for signs of liver cancer.
- You may be prescribed medications to help reduce the buildup of toxins in your blood due to poor liver function.
Liver transplant surgery
In advanced cases of cirrhosis, when the liver ceases to function, a liver transplant may be the only treatment option. A liver transplant is a procedure to replace your liver with a healthy liver from a deceased donor or with part of a liver from a living donor.
Preventive measures
Reduce your risk of cirrhosis by taking these steps to care for your liver:
- Do not drink alcohol if you have cirrhosis
- Eat a healthy diet
- Maintain a healthy weight
- Reduce your risk of hepatitis
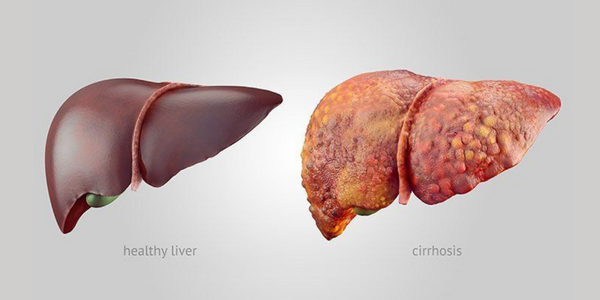
What is liver abscess
A liver abscess is a pocket of pus that forms in the liver due to a bacterial infection. In the case of liver abscess, instead of draining from the infection site, the pus collects in a pocket inside the liver. An abscess is usually accompanied by swelling and inflammation in the surrounding area. It can cause pain and swelling in the abdomen.
Causes
The most common cause is biliary disease. This is a broad term for conditions in the biliary tree affecting the liver, pancreas, and gallbladder.
Other causes and risk factors include:
- bacteria from a ruptured appendix that forms an abscess
- pancreatic cancer
- colon cancer
- inflammatory bowel disease, such as diverticulitis or a perforated bowel
- a blood infection, or septicemia
- trauma to the liver by accident or injury
Symptoms
PLA symptoms resemble those of gallbladder inflammation or massive infection. They may include:
- chills
- vomiting
- fever
- right upper abdominal pain
- sudden dramatic weight loss, such as 10 pounds in a few weeks
- dark-colored urine
- whitish or grey, clay-colored stool
- Diarrhea
Treatment
A combination of blood cultures and imaging tests to diagnose the condition may be used:
- an abdominal ultrasound to locate an abscess
- a CT scan with intravenous contrast, or injected dye, to find and measure the abscess
- blood tests to look for signs of infectious inflammation, such as an increased serum white blood count and neutrophil level
- blood cultures for bacterial growth to determine which antibiotic(s) you need
- an MRI of the abdomen
A liver abscess may appear as a mass containing gas and fluid in the liver when viewed with CT scans.
Some people can be successfully treated with antibiotics alone. Most, however, need drainage of the abscess, which is considered to be the ideal therapy. This involves inserting a needle and possibly placing a drainage catheter into the abscess to remove the infection-containing pus. A liver biopsy might be performed at the same time by taking a sample of your liver tissue. This helps determine the overall health of your liver.
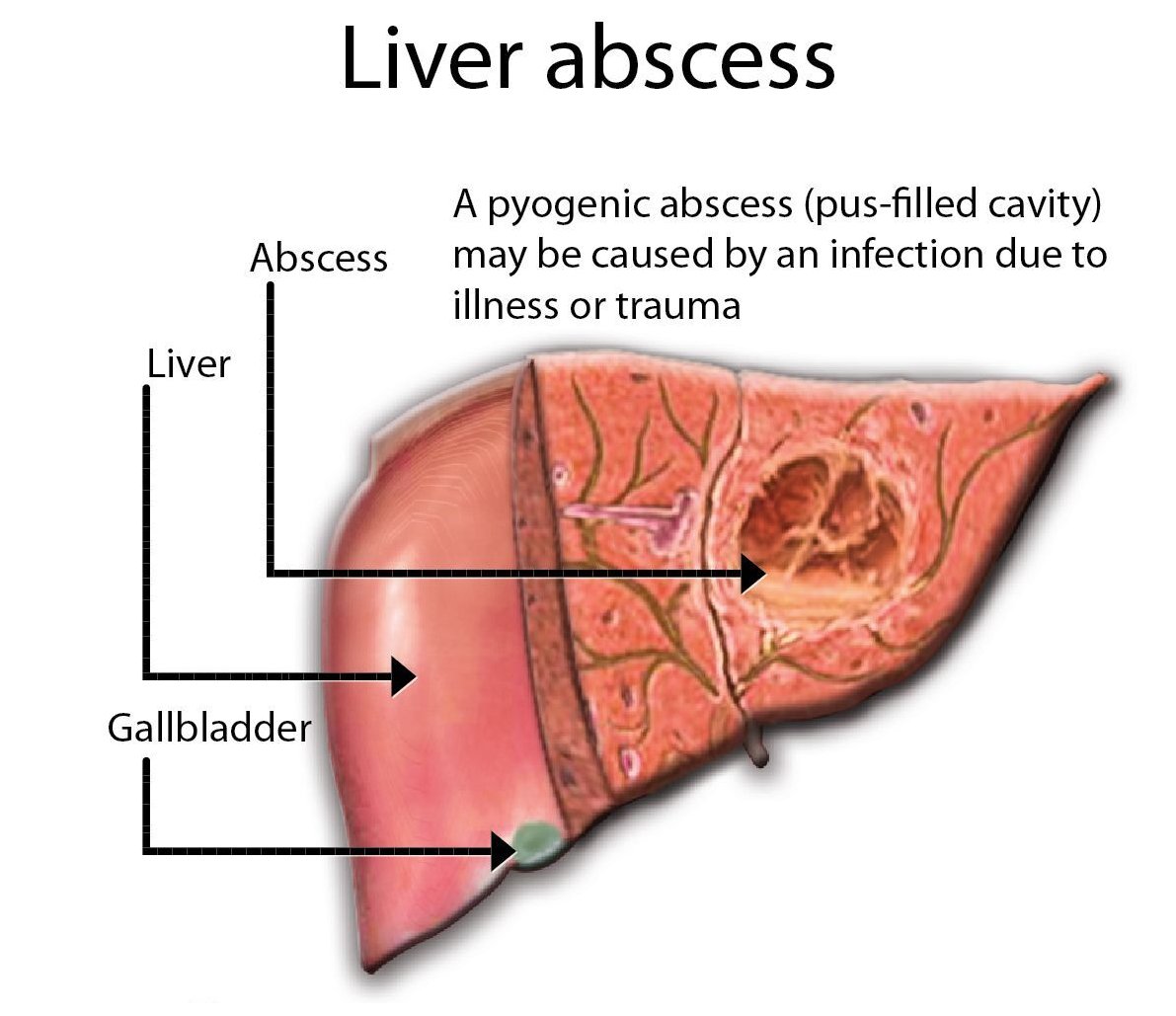
What is liver cancer
Liver cancer is cancer that begins in the cells of your liver. Your liver is a football-sized organ that sits in the upper right portion of your abdomen, beneath your diaphragm and above your stomach.
Several types of cancer can form in the liver. The most common type of liver cancer is hepatocellular carcinoma, which begins in the main type of liver cell (hepatocyte). Other types of liver cancer, such as intrahepatic cholangiocarcinoma and hepatoblastoma, are much less common.
Causes
Liver cancer happens when liver cells develop changes (mutations) in their DNA. DNA mutations cause changes in these instructions. One result is that cells may begin to grow out of control and eventually form a tumor — a mass of cancerous cells.Factors that increase the risk of primary liver cancer include:
- Chronic infection with HBV or HCV
- Cirrhosis. This progressive and irreversible condition causes scar tissue to form in your liver and increases your chances of developing liver cancer.
- Certain inherited liver diseases
- Diabetes
- Nonalcoholic fatty liver disease
- Exposure to aflatoxins. Aflatoxins are poisons produced by molds that grow on crops that are stored poorly.
- Excessive alcohol consumption
Symptoms
When signs and symptoms do appear, they may include:
- Losing weight without trying
- Loss of appetite
- Upper abdominal pain
- Nausea and vomiting
- General weakness and fatigue
- Abdominal swelling
- Jaundice
- White, chalky stools
Treatment
Tests and procedures used to diagnose liver cancer include:
- Blood tests
- Imaging tests. Recommended imaging tests, such as an ultrasound, CT and MRI.
- Removing a sample of liver tissue for testing. Sometimes it's necessary to remove a piece of liver tissue for laboratory testing in order to make a definitive diagnosis of liver cancer.
Treatments for primary liver cancer depend on the extent (stage) of the disease as well as your age, overall health and personal preferences.
Surgery
Operations used to treat liver cancer include:
- Surgery to remove the tumor. It will recommend an operation to remove the liver cancer and a small portion of healthy liver tissue that surrounds it if your tumor is small and your liver function is good.
- Liver transplant surgery. During liver transplant surgery, your diseased liver is removed and replaced with a healthy liver from a donor. Localized treatments
Localized treatment options for liver cancer include:
- Heating cancer cells. Radiofrequency ablation uses electric current to heat and destroy cancer cells.
- Freezing cancer cells. Cryoablation uses extreme cold to destroy cancer cells.
- Injecting alcohol into the tumor. During alcohol injection, pure alcohol is injected directly into tumors, either through the skin or during an operation.
- Injecting chemotherapy drugs into the liver.
- Placing beads filled with radiation in the liver. Tiny spheres that contain radiation may be placed directly in the liver where they can deliver radiation directly to the tumor.
Radiation therapy
This treatment uses high-powered energy from sources such as X-rays and protons to destroy cancer cells and shrink tumors. Radiation therapy might be an option if other treatments aren't possible or if they haven't helped. For advanced liver cancer, radiation therapy might help control symptoms.
Targeted drug therapy
Targeted drug treatments focus on specific abnormalities present within cancer cells. By blocking these abnormalities, targeted drug treatments can cause cancer cells to die.
Immunotherapy
Immunotherapy uses your immune system to fight cancer. Your body's disease-fighting immune system may not attack your cancer because the cancer cells produce proteins that blind the immune system cells. Immunotherapy works by interfering with that process.
Chemotherapy
Chemotherapy uses drugs to kill rapidly growing cells, including cancer cells. Chemotherapy can be administered through a vein in your arm, in pill form or both.
Preventive measures
- Reduce your risk of cirrhosis
- Drink alcohol in moderation, if at all.
- Maintain a healthy weight.
- Get vaccinated against hepatitis B
- Take measures to prevent hepatitis C
- Seek treatment for hepatitis B or C infection
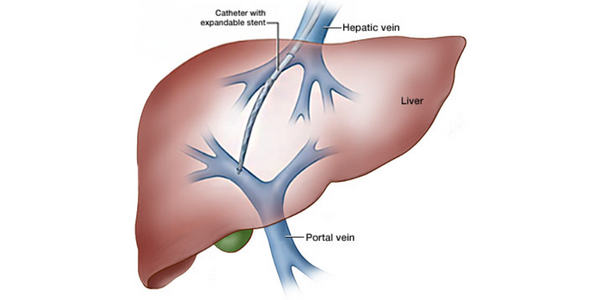
What is portal hypertension
Portal hypertension is an increase in the blood pressure within a system of veins called the portal venous system. Veins coming from the stomach, intestine, spleen, and pancreas merge into the portal vein, which then branches into smaller vessels and travels through the liver. If the vessels in the liver are blocked due to liver damage, blood cannot flow properly through the liver. As a result, high pressure in the portal system develops. This increased pressure in the portal vein may lead to the development of large, swollen veins (varices) within the esophagus, stomach, rectum, or umbilical area (belly button).
Causes
The most common cause of portal hypertension is cirrhosis of the liver. Cirrhosis is scarring which accompanies the healing of liver injury caused by hepatitis, alcohol, or other less common causes of liver damage. In cirrhosis, the scar tissue blocks the flow of blood through the liver.
Other causes of portal hypertension include blood clots in the portal vein, blockages of the veins that carry the blood from the liver to the heart, a parasitic infection called schistosomiasis, and focal nodular hyperplasia, a disease seen in people infected with HIV, the virus that may lead to AIDS.
Symptoms
The main symptoms and complications of portal hypertension include:
- Gastrointestinal bleeding marked by black, tarry stools or blood in the stools, or vomiting of blood due to the spontaneous rupture and hemorrhage from varices
- Ascites (an accumulation of fluid in the abdomen)
- Encephalopathy or confusion and forgetfulness caused by poor liver function
- Reduced levels of platelets, blood cells that help form blood clots, or white blood cells, the cells that fight infection
Treatment
Usually, the diagnosis of portal hypertension is based on the presence of ascites or of dilated veins or varices as seen during a physical exam of the abdomen or the anus. Various lab tests, X-ray tests, and endoscopic exams may also be used. Treatment focuses on preventing or managing the complications, especially the bleeding from the varices.Treatment may include:
- Endoscopic therapy This is usually the first line of treatment for variceal bleeding and consists of either banding or sclerotherapy. Banding is a procedure in which a gastroenterologist uses rubber bands to block off the blood vessel to stop bleeding. Sclerotherapy is occasionally used when banding cannot be used and is a procedure in which a blood-clotting solution is injected into the bleeding varices to stop bleeding.
- Medications Nonselective beta-blockers may be prescribed alone or in combination with endoscopic therapy to reduce the pressure in varices and further reduce the risk of bleeding. Nonselective beta blockers are also prescribed to prevent a first variceal hemorrhage in a patient with varices that are felt to be at risk for bleeding. Esophageal variceal banding has also been used for that purpose, especially in patients who can't take beta blockers.
Other Treatments for Portal Hypertension
- Liver transplantThis is done in cases of end-stage liver disease.
- Devascularization A surgical procedure that removes the bleeding varices; this procedure is done when a TIPS or a surgical shunt is not possible or is unsuccessful in controlling the bleeding.
- ParacentesisThis is a procedure in which the accumulation of fluid in the abdomen (ascites) is directly removed. The results are usually temporary and the procedure will need to be repeated as needed.
Preventive measures
Some of the things you can do to improve the function of your liver include the following:
- Do not use alcohol or street drugs.
- Do not take any over-the-counter or prescription drugs or herbal medicines without first consulting your doctor or nurse
- Follow the dietary guidelines given by your healthcare provider, including eating a low-sodium (salt) diet.
What is liver infections
Your liver does a lot of things that keep you healthy. It turns nutrients into chemicals your body needs. It filters out poisons. It helps turn food into energy. So when your liver doesn’t work well, that can affect your whole body. Parasites and viruses can infect the liver, causing inflammation that reduces liver function. The viruses that cause liver damage can be spread through blood or semen, contaminated food or water, or close contact with a person who is infected. The most common types of liver infection are hepatitis viruses, including:
- Hepatitis A
- Hepatitis B
- Hepatitis C
Causes
You usually get it when you eat or drink something that's got the virus in it. Hepatitis B spreads in several ways.You can get it from sex with someone who's sick or by sharing a needle when using street drugs. The virus also can pass from mothers to their newborn child at birth or soon afterward. You get hepatitis C if you have contact with contaminated blood or needles used to inject illegal drugs or draw tattoos.
Symptoms
You usually get it when you eat or drink something that's got the virus in it. Hepatitis B spreads in several ways.You can get it from sex with someone who's sick or by sharing a needle when using street drugs. The virus also can pass from mothers to their newborn child at birth or soon afterward. You get hepatitis C if you have contact with contaminated blood or needles used to inject illegal drugs or draw tattoos.
Common symptoms of infectious hepatitis include:
- Fatigue
- flu-like symptoms
- dark urine
- pale stool
- abdominal pain
- loss of appetite
- unexplained weight loss
- yellow skin and eyes, which may be signs of jaundice
Treatment
It is crucial to understand what is causing hepatitis in order to treat it correctly.
- History and physical exam: To diagnose all forms of hepatitis, your history will determine any risk factors you may have. During a physical examination, your abdomen will be pressed down gently to see if there’s pain or tenderness. Any swelling of the liver and any yellow discoloration in your eyes or skin will also be checked for.
- Liver function tests: Liver function tests use blood samples to determine how efficiently your liver works.Abnormal results of these tests may be the first indication that there is a problem, especially if you don’t show any signs on a physical exam of liver disease.
- Other blood tests: If your liver function tests are abnormal, other blood tests will be done to detect the source of the problem. These tests can determine if you have infectious hepatitis by checking for the presence of hepatitis viruses or antibodies your body produces to combat them.Doctors may also use blood tests to check for any signs of autoimmune hepatitis.
- Liver biopsy: When diagnosing hepatitis, potential damage of your liver will also be assessed. A liver biopsy is a procedure that involves taking a sample of tissue from your liver. This test will determine how infection or inflammation has affected your liver.
- Ultrasound: An abdominal ultrasound uses ultrasound waves to create an image of the organs within your abdomen. It can reveal:
- fluid in your abdomen
- liver damage or enlargement
- liver tumors
- abnormalities of your gallbladder
How hepatitis is treated
Treatment options will vary by the type of hepatitis you have and whether the infection is acute or chronic.
- Hepatitis A: Hepatitis A is a short-term illness and may not require treatment. However, if symptoms cause a great deal of discomfort, bed rest may be necessary. In addition, if you experience vomiting or diarrhea, a dietary program to maintain your hydration and nutrition will be recommended.
- Hepatitis B: There is no specific treatment program for acute hepatitis B. However, if you have chronic hepatitis B, you will require antiviral medications. This form of treatment can be costly, as you may have to continue it for several months or years. Treatment for chronic hepatitis B also requires regular medical evaluations and monitoring to determine if the virus is responding to treatment.
- Hepatitis C: Antiviral medications can treat both acute and chronic forms of hepatitis C. Typically, people who develop chronic hepatitis C will use a combination of antiviral drug therapies. They may also need further testing to determine the best form of treatment. People who develop cirrhosis or liver disease due to chronic hepatitis C may be candidates for a liver transplant.
Preventive measures
To prevent liver infection:
- Drink alcohol in moderation
- Avoid risky behavior
- Get vaccinated
- Use medications wisely
- Avoid contact with other people's blood and body fluids
- Keep your food safe
- Take care with aerosol sprays
- Protect your skin
- Maintain a healthy weight