GI cancers
Information you need to understand your disease and the tests you may need.
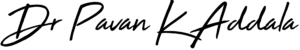
What is Esophageal cancer
Esophageal cancer occurs when cancer cells develop in the esophagus, a tube-like structure that runs from your throat to your stomach. Food goes from the mouth to the stomach through the esophagus. The cancer starts at the inner layer of the esophagus and can spread throughout the other layers of the esophagus and to other parts of the body (metastasis).
Causes
It's not exactly clear what causes esophageal cancer. Esophageal cancer occurs when cells in the esophagus develop changes (mutations) in their DNA. The changes make cells grow and divide out of control. The accumulating abnormal cells form a tumor in the esophagus that can grow to invade nearby structures and spread to other parts of the body.
Factors that cause irritation in the cells of your esophagus and increase your risk of esophageal cancer include:
- Having gastroesophageal reflux disease (GERD)
- Smoking
- Having precancerous changes in the cells of the esophagus (Barrett's esophagus)
- Being obese
- Drinking alcohol
- Having bile reflux
- Having difficulty swallowing because of an esophageal sphincter that won't relax (achalasia)
- Having a steady habit of drinking very hot liquids
- Not eating enough fruits and vegetables
- Undergoing radiation treatment to the chest or upper abdomen
Symptoms
Signs and symptoms of esophageal cancer include:
- Difficulty swallowing (dysphagia)
- Weight loss without trying
- Chest pain, pressure or burning
- Worsening indigestion or heartburn
- Coughing or hoarseness
Early esophageal cancer typically causes no signs or symptoms.
Treatment
To diagnose esophageal cancer, your doctor will review your symptoms, medical history, and examine you. In addition, they may order certain blood tests and X-rays. Tests for esophageal cancer may include:
- Barium swallows X-ray, in which you drink a liquid that coats your esophagus. This makes the esophagus stand out on the X-ray so that your doctor can identify certain problems.
- Endoscopy: the doctor passes an endoscope, a thin, lighted tube, down your throat into your esophagus to examine it. Endoscopic ultrasound uses sound waves to provide more information about the extent of tumor involvement in nearby tissues.
- Biopsy: during an endoscopy, the doctor can take cells or tissue from your esophagus. The cells are examined under a microscope for the presence of cancer.
Other tests, including computed tomography (CT) scans, positron emission tomography (PET) scan, thoracoscopy, and laparoscopy, may be performed to determine if the cancer has spread, or metastasized, outside of the esophagus. This process is called "staging." The doctor needs this information in order to plan your treatment.
Treatment of esophageal cancer depends on many factors, including the stage of the cancer and the overall health of the patient.
- Surgery. Part or all of the esophagus may be removed.
- Radiation therapy. Kills cancer cells with radiation.
- Chemotherapy. Powerful drugs that attack cancer cells throughout the body; typically used in combination with radiation therapy and/or surgery.
- Targeted therapy. Newer treatments that target specific aspects of a cancer to curb cancer growth and spread.
- Immunotherapy. Helps the immune system to attack cancer cells.
- Photodynamic therapy. Targets cancer cells with a special laser light.
- Electrocoagulation. Uses electric current to destroy cancer cells.
- Cryotherapy. Freezes cancer cells to help shrink a tumor.
Endoscopic mucosal resection may be done to treat precancers or very small early cancers by removing the inner lining of the esophagus. Radiofrequency ablation treatment using a device that targets cancer cells with radiofrequency energy is sometimes used for early cancers.
Preventive measures
You can take steps to reduce your risk of esophageal cancer. For instance:
- Quit smoking. If you smoke, talk to your doctor about strategies for quitting. Medications and counseling are available to help you quit. If you don't use tobacco, don't start.
- Drink alcohol in moderation, if at all. If you choose to drink alcohol, do so in moderation. For healthy adults, that means up to one drink a day for women and up to two drinks a day for men.
- Eat more fruits and vegetables. Add a variety of colorful fruits and vegetables to your diet.
- Maintain a healthy weight. If you are overweight or obese, talk to your doctor about strategies to help you lose weight. Aim for a slow and steady weight loss of 1 or 2 pounds a week.
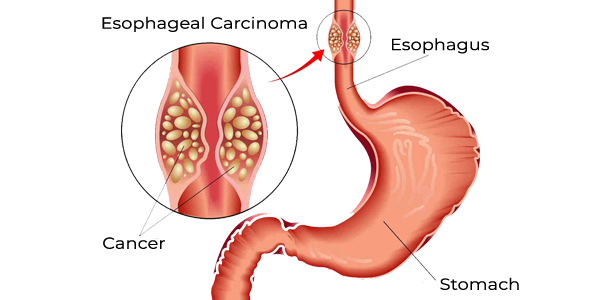
What is liver cancer
Liver cancer is cancer that begins in the cells of your liver. Your liver is a football-sized organ that sits in the upper right portion of your abdomen, beneath your diaphragm and above your stomach.
Several types of cancer can form in the liver. The most common type of liver cancer is hepatocellular carcinoma, which begins in the main type of liver cell (hepatocyte). Other types of liver cancer, such as intrahepatic cholangiocarcinoma and hepatoblastoma, are much less common.
Causes
Liver cancer happens when liver cells develop changes (mutations) in their DNA. DNA mutations cause changes in these instructions. One result is that cells may begin to grow out of control and eventually form a tumor — a mass of cancerous cells.Factors that increase the risk of primary liver cancer include:
- Chronic infection with HBV or HCV
- Cirrhosis. This progressive and irreversible condition causes scar tissue to form in your liver and increases your chances of developing liver cancer.
- Certain inherited liver diseases
- Diabetes
- Nonalcoholic fatty liver disease
- Exposure to aflatoxins. Aflatoxins are poisons produced by molds that grow on crops that are stored poorly.
- Excessive alcohol consumption
Symptoms
When signs and symptoms do appear, they may include:
- Losing weight without trying
- Loss of appetite
- Upper abdominal pain
- Nausea and vomiting
- General weakness and fatigue
- Abdominal swelling
- Jaundice
- White, chalky stools
Treatment
Tests and procedures used to diagnose liver cancer include:
- Blood tests
- Imaging tests. Recommended imaging tests, such as an ultrasound, CT and MRI.
- Removing a sample of liver tissue for testing. Sometimes it's necessary to remove a piece of liver tissue for laboratory testing in order to make a definitive diagnosis of liver cancer.
Treatments for primary liver cancer depend on the extent (stage) of the disease as well as your age, overall health and personal preferences.
Surgery
Operations used to treat liver cancer include:
- Surgery to remove the tumor. It will recommend an operation to remove the liver cancer and a small portion of healthy liver tissue that surrounds it if your tumor is small and your liver function is good.
- Liver transplant surgery. During liver transplant surgery, your diseased liver is removed and replaced with a healthy liver from a donor. Localized treatments
Localized treatment options for liver cancer include:
- Heating cancer cells. Radiofrequency ablation uses electric current to heat and destroy cancer cells.
- Freezing cancer cells. Cryoablation uses extreme cold to destroy cancer cells.
- Injecting alcohol into the tumor. During alcohol injection, pure alcohol is injected directly into tumors, either through the skin or during an operation.
- Injecting chemotherapy drugs into the liver.
- Placing beads filled with radiation in the liver. Tiny spheres that contain radiation may be placed directly in the liver where they can deliver radiation directly to the tumor.
Radiation therapy
This treatment uses high-powered energy from sources such as X-rays and protons to destroy cancer cells and shrink tumors. Radiation therapy might be an option if other treatments aren't possible or if they haven't helped. For advanced liver cancer, radiation therapy might help control symptoms.
Targeted drug therapy
Targeted drug treatments focus on specific abnormalities present within cancer cells. By blocking these abnormalities, targeted drug treatments can cause cancer cells to die.
Immunotherapy
Immunotherapy uses your immune system to fight cancer. Your body's disease-fighting immune system may not attack your cancer because the cancer cells produce proteins that blind the immune system cells. Immunotherapy works by interfering with that process.
Chemotherapy
Chemotherapy uses drugs to kill rapidly growing cells, including cancer cells. Chemotherapy can be administered through a vein in your arm, in pill form or both.
Preventive measures
- Reduce your risk of cirrhosis
- Drink alcohol in moderation, if at all.
- Maintain a healthy weight.
- Get vaccinated against hepatitis B
- Take measures to prevent hepatitis C
- Seek treatment for hepatitis B or C infection
What is gallbladder cancer
Gallbladder cancer is an abnormal growth of cells that begins in the gallbladder. Your gallbladder is a small, pear-shaped organ on the right side of your abdomen, just beneath your liver. The gallbladder stores bile, a digestive fluid produced by your liver.
When gallbladder cancer is discovered at its earliest stages, the chance for a cure is very good. Gallbladder cancer may not be discovered until it's advanced because it often causes no specific signs or symptoms. Also, the relatively hidden nature of the gallbladder makes it easier for gallbladder cancer to grow without being detected.
Causes
Gallbladder cancer forms when healthy gallbladder cells develop changes (mutations) in their DNA. The changes tell the cells to grow out of control and to continue living when other cells would normally die. The accumulating cells form a tumor that can grow beyond the gallbladder and spread to other areas of the body.
Most gallbladder cancer begins in the glandular cells that line the inner surface of the gallbladder. Gallbladder cancer that begins in this type of cell is called adenocarcinoma.
Symptoms
Gallbladder cancer signs and symptoms may include:
- Abdominal pain, particularly in the upper right portion of the abdomen
- Abdominal bloating
- Losing weight without trying
- Yellowing of the skin and whites of the eyes (jaundice)
Treatment
Tests and procedures used to diagnose gallbladder cancer include:
- Blood tests. Blood tests to evaluate your liver function & what's causing your signs and symptoms.
- Procedures to create images of the gallbladder. Imaging tests that can create pictures of the gallbladder include ultrasound, computerized tomography (CT) and magnetic resonance imaging (MRI).
Your gallbladder cancer's stage helps determine your prognosis and your treatment options. Tests and procedures used to stage gallbladder cancer include:
- Exploratory surgery. Laparoscopy surgery by making a small incision & insert a tiny camera to look inside your abdomen for signs that gallbladder cancer has spread.
- Tests to examine the bile ducts. Procedures to inject dye into the bile ducts. This is followed by an imaging test that records where the dye goes. These tests can show blockages in the bile ducts.
- These tests may include magnetic resonance cholangiography and endoscopic retrograde cholangiopancreatography (ERCP).
- Additional imaging tests. Most people with gallbladder cancer will undergo a series of scans to help determine whether the cancer has spread or remains localized. Which scans should be performed vary depending on your circumstances. Common scans include a CT and MRI scans of the abdomen and chest.
The stages of gallbladder cancer range from 0 to IV. The earliest stages indicate a cancer that's confined to the gallbladder. Later stages indicate more-advanced cancer that has grown to involve nearby organs or has spread to other areas of the body.
Surgery for early-stage gallbladder cancer
- Surgery to remove the gallbladder. Early gallbladder cancer that is confined to the gallbladder is treated with an operation to remove the gallbladder (cholecystectomy).
- Surgery to remove the gallbladder and a portion of the liver. Gallbladder cancer that extends beyond the gallbladder and into the liver is sometimes treated with surgery to remove the gallbladder, as well as portions of the liver and bile ducts that surround the gallbladder.
If your gallbladder cancer is very small and can be removed completely with cholecystectomy, you may not need additional treatments. If there's a risk that cancer cells may remain after surgery, chemotherapy or other treatments might be suggested.
Chemotherapy
Chemotherapy uses drugs to kill rapidly growing cells, including cancer cells. Chemotherapy can be administered through a vein in your arm, in pill form or both.
Radiation therapy
Radiation therapy uses high-powered beams of energy, such as X-rays and protons, to kill cancer cells. The energy beams come from a machine that moves around you as you lie on a table.
Targeted drug therapy
Targeted drug treatments focus on specific weaknesses present within cancer cells. By blocking these weaknesses, targeted drug treatments can cause cancer cells to die. Targeted drugs might be an option for people with advanced gallbladder cancer.
Immunotherapy
Immunotherapy is a drug treatment that helps your immune system to fight cancer. Your body's disease-fighting immune system might not attack cancer because the cancer cells produce proteins that make it hard for the immune system cells to recognize the cancer cells as dangerous. Immunotherapy works by interfering with that process.
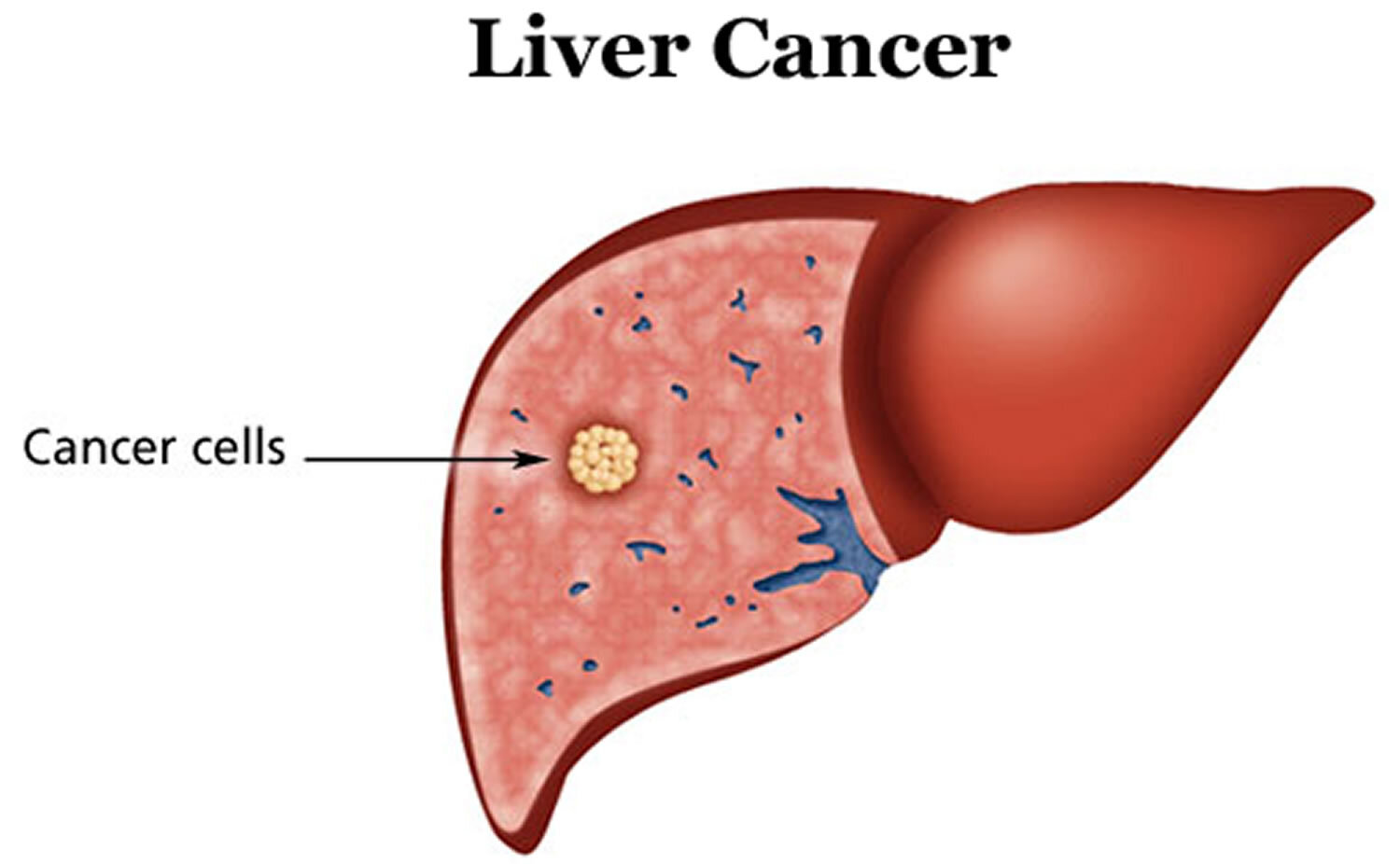
What is Pancreatic Cancer
Pancreatic cancer begins in the tissues of your pancreas — an organ in your abdomen that lies behind the lower part of your stomach. Your pancreas releases enzymes that aid digestion and produces hormones that help manage your blood sugar.
Several types of growths can occur in the pancreas, including cancerous and noncancerous tumors. The most common type of cancer that forms in the pancreas begins in the cells that line the ducts that carry digestive enzymes out of the pancreas (pancreatic ductal adenocarcinoma).
Pancreatic cancer treatment options are chosen based on the extent of the cancer. Options may include surgery, chemotherapy, radiation therapy or a combination of these.
Causes
Pancreatic cancer occurs when cells in your pancreas develop changes (mutations) in their DNA. A cell's DNA contains the instructions that tell a cell what to do. These mutations tell the cells to grow uncontrollably and to continue living after normal cells would die. These accumulating cells can form a tumor. When left untreated, the pancreatic cancer cells can spread to nearby organs and blood vessels and to distant parts of the body.
Most pancreatic cancer begins in the cells that line the ducts of the pancreas. This type of cancer is called pancreatic adenocarcinoma or pancreatic exocrine cancer. Less frequently, cancer can form in the hormone-producing cells or the neuroendocrine cells of the pancreas. These types of cancer are called pancreatic neuroendocrine tumors, islet cell tumors or pancreatic endocrine cancer.
Factors that may increase your risk of pancreatic cancer include:
- Smoking
- Diabetes
- Chronic inflammation of the pancreas (pancreatitis)
- Family history of genetic syndromes that can increase cancer risk, Family history of pancreatic cancer
- Obesity
- Older age, as most people are diagnosed after age 65
Symptoms
Signs and symptoms of pancreatic cancer often don't occur until the disease is advanced. They may include:
- Abdominal pain that radiates to your back
- Loss of appetite or unintended weight loss
- Yellowing of your skin and the whites of your eyes (jaundice)
- Light-colored stools
- Dark-colored urine
- Itchy skin
- New diagnosis of diabetes or existing diabetes that's becoming more difficult to control
- Blood clots
- Fatigue
Treatment
In addition to a history and physical exam, imaging tests will be performed to help make the diagnosis of pancreatic cancer. These tests include:
- Ultrasound
- CT scanning
- MRI
- Endoscopic ultrasonography
- Endoscopic retrograde cholangiopancreatography (ERCP)
A definitive diagnosis of pancreatic cancer only comes from removal of tissue (biopsy) for examination in a lab. This can be done with a needle through the skin, during endoscopy, or with an operation.
Pancreatic cancer is treated in several ways, alone or in combination: Surgery
- Chemotherapy
- Immunotherapy
- Radiation therapy
- Targeted therapy
- Palliative care
Surgery is generally done to attempt to cure pancreatic cancer, but it may also be done to lessen or prevent symptoms. Chemotherapy and radiation are often given together, prior to, after, or even without surgery, to slow pancreatic cancer's growth. Targeted therapy is sometimes given to treat advanced pancreatic cancer. Immunotherapy can be given to people whose cancer cells have certain gene changes.Palliative care aims to reduce discomfort for people whose pancreatic cancer cannot be cured.
Preventive measures
You may reduce your risk of pancreatic cancer if you:
- Stop smoking
- Maintain a healthy weight
- Choose a healthy diet
What is colorectal cancer
Colon cancer is a type of cancer that begins in the large intestine (colon). The colon is the final part of the digestive tract. Colon cancer typically affects older adults, though it can happen at any age. It usually begins as small, noncancerous (benign) clumps of cells called polyps that form on the inside of the colon. Over time some of these polyps can become colon cancers. If colon cancer develops, many treatments are available to help control it, including surgery, radiation therapy and drug treatments, such as chemotherapy, targeted therapy and immunotherapy.

Causes
In general, colon cancer begins when healthy cells in the colon develop changes (mutations) in their DNA. A cell's DNA contains a set of instructions that tell a cell what to do. Healthy cells grow and divide in an orderly way to keep your body functioning normally. But when a cell's DNA is damaged and becomes cancerous, cells continue to divide — even when new cells aren't needed. As the cells accumulate, they form a tumor. With time, the cancer cells can grow to invade and destroy normal tissue nearby. And cancerous cells can travel to other parts of the body to form deposits there (metastasis)
There are several types of colorectal cancer, based on where it starts
- Adenocarcinoma. This is the most common kind, making up 96% of cases. It starts in cells that make mucus for your colon and rectum.
- Carcinoid tumor. This begins in cells that make hormones.
- Gastrointestinal stromal tumor. This forms in cells in the wall of your colon that tell your gastrointestinal muscles to move food or liquid along.
- Lymphoma. This is cancer of your immune system cells.
- Sarcoma. This starts in connective tissues like blood vessels or muscle layers.
Nearly all colon and rectal cancers begin as a polyp, a growth on the inner surface of your colon. Polyps themselves usually aren’t cancer.
- Hyperplastic and inflammatory polyps. These usually don’t carry a chance of cancer. But large hyperplastic polyps, especially on the right side of your colon, can be a problem. Your doctor will want to remove them.
- Adenomas or adenomatous polyps. These are precancerous. If you leave them alone, they could turn into colon cancer
Symptoms
Signs and symptoms of colon cancer include:
- A persistent change in your bowel habits, including diarrhea or constipation or a change in the consistency of your stool
- Rectal bleeding or blood in your stool
- Persistent abdominal discomfort, such as cramps, gas or pain
- A feeling that your bowel doesn't empty completely
- Weakness or fatigue
- Unexplained weight loss
Colorectal Cancer Diagnosis
- Rectal exam. Your doctor can use their fingers to feel for growths.
- Colonoscopy. This is the standard screening test that experts recommend. Your doctor uses a thin, flexible tube called a colonoscope to look at your entire colon and rectum.
- Sigmoidoscopy. Your doctor looks at your rectum and the last part of your colon.
- Biopsy. Your doctor may take out a bit of tissue during a colonoscopy or sigmoidoscopy and send it to a lab for testing. They can also use a needle to take a sample, with a CT scan or ultrasound to guide them. Complications are rare, but you may have some bleeding or discomfort.
- Stool DNA. This test looks for certain gene changes that might be a sign of colon cancer.
- CT colonography. This is a special X-ray (also called a virtual colonoscopy) of your entire colon. It takes less time and is less invasive than other tests. But if it shows a polyp, you’ll still need a colonoscopy.
- Barium enema X-ray. This is a type of X-ray that involves putting dye in your colon. It can find trouble spots that might mean you need a colonoscopy.
- Other imaging tests. MRI or ultrasound can give your doctor a better look at your organs.
Treatment
Which treatments are most likely to help you depends on your particular situation, including the location of your cancer, its stage and your other health concerns.
Surgery for early-stage colon cancer
- polyps during a colonoscopy (polypectomy) If your cancer is small, localized, completely contained within a polyp and in a very early stage, your doctor may be able to remove it completely during a colonoscopy.
- Endoscopic mucosal resection Larger polyps might be removed during colonoscopy using special tools to remove the polyp and a small amount of the inner lining of the colon in a procedure called an endoscopic mucosal resection.
- Minimally invasive surgery (laparoscopic surgery) Polyps that can't be removed during a colonoscopy may be removed using laparoscopic surgery. In this procedure, your surgeon performs the operation through several small incisions in your abdominal wall, inserting instruments with attached cameras that display your colon on a video monitor.
Surgery for more advanced colon cancer
- Partial colectomy During this procedure, the surgeon removes the part of your colon that contains the cancer, along with a margin of normal tissue on either side of the cancer. This procedure can commonly be done by a minimally invasive approach (laparoscopy).
- Surgery to create a way for waste to leave your body When it's not possible to reconnect the healthy portions of your colon or rectum, you may need an ostomy. This involves creating an opening in the wall of your abdomen from a portion of the remaining bowel for the elimination of stool into a bag that fits securely over the opening.
- Lymph node removal Nearby lymph nodes are usually also removed during colon cancer surgery and tested for cancer.
Surgery for advanced cancer
If your cancer is very advanced or your overall health very poor, we may recommend an operation to relieve a blockage of your colon or other conditions in order to improve your symptoms.
Chemotherapy
Chemotherapy uses drugs to destroy cancer cells. Chemotherapy for colon cancer is usually given after surgery if the cancer is larger or has spread to the lymph nodes. In this way, chemotherapy may kill any cancer cells that remain in the body and help reduce the risk of cancer recurrence
Chemotherapy might also be used before an operation to shrink a large cancer so that it's easier to remove with surgery
Chemotherapy can also be used to relieve symptoms of colon cancer that can't be removed with surgery or that has spread to other areas of the body. Sometimes it's combined with radiation therapy.
Radiation therapy
Radiation therapy uses powerful energy sources, such as X-rays and protons, to kill cancer cells. It might be used to shrink a large cancer before an operation so that it can be removed more easily. When surgery isn't an option, radiation therapy might be used to relieve symptoms, such as pain.
Targeted drug therapy
Targeted drug treatments focus on specific abnormalities present within cancer cells. By blocking these abnormalities, targeted drug treatments can cause cancer cells to die. Targeted drugs are usually combined with chemotherapy.
Immunotherapy
Immunotherapy is a drug treatment that uses your immune system to fight cancer. Your body's disease-fighting immune system may not attack your cancer because the cancer cells produce proteins that blind the immune system cells from recognizing the cancer cells. Immunotherapy works by interfering with that process.
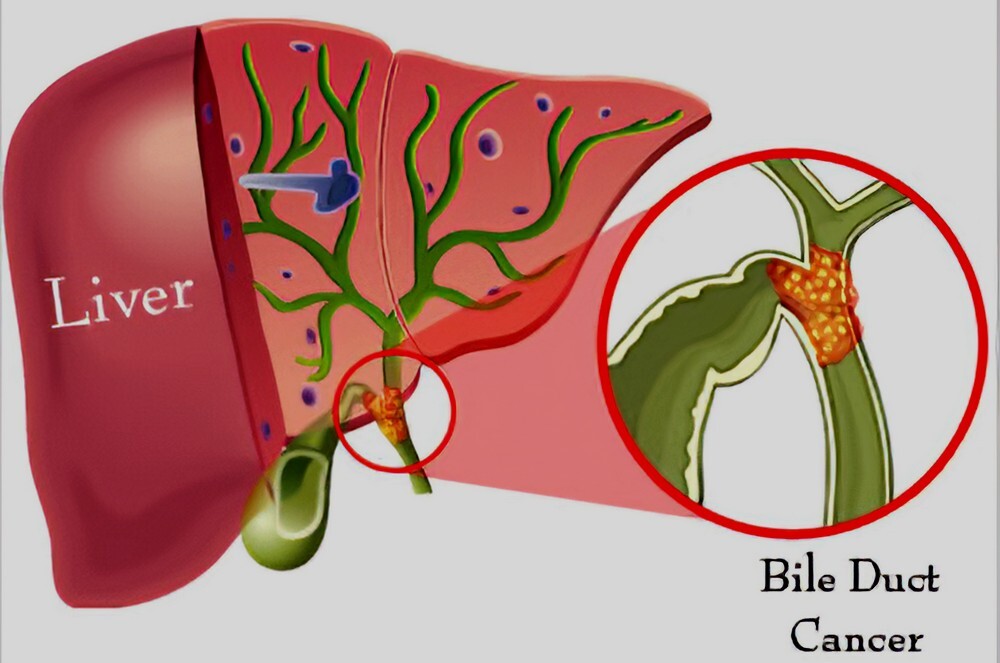
What is bile duct cancer
Bile duct cancer, also called cholangiocarcinoma, is when unusual cells grow out of control inside your bile ducts. Those are thin tubes about 4 to 5 inches long that move a fluid called bile from your liver to your gallbladder and small intestine. Bile helps you digest fat in the food you eat.
Bile duct cancer can be identified based on where it starts:
Outside your liver (extrahepatic). This type occurs more often and is more treatable. Cancer might form in one of two areas.
- The hilum region, where your left and right bile ducts come together to form the common hepatic duct. This is called perihilar cancer.
- The distal region, where your common bile duct passes through your pancreas. This is called distal cancer.
Inside your liver (intrahepatic). This type makes up 5% to 10% of cases.
Causes
Certain things can raise your chances of getting it, including long-term inflammation from conditions including:
- Primary sclerosing cholangitis: This inflammation of your bile duct leads to scarring. Many people who have it also have ulcerative colitis, an inflammation of the large intestine.
- Bile duct stones. These are similar to gallstones but much smaller.
- Choledochal cysts: Some people are born with a rare condition that causes bile-filled sacs along your bile ducts. Without treatment, they may lead to bile duct cancer.
- Liver fluke infection: It happens when people eat raw or poorly cooked fish that’s infected with tiny parasitic worms called liver flukes. They can live in your bile ducts and cause cancer.
- Reflux: When digestive juices from your pancreas flow back into your bile ducts, they can’t empty properly.
- Cirrhosis: Alcohol and hepatitis can damage your liver and cause scar tissue, raising the risk of bile duct cancer.
Other things that can make you more likely to get bile duct cancer include:
- Inflammatory bowel disease (including Crohn’s disease and ulcerative colitis)
- Obesity
- Diabetes
- Viral hepatitis
- Drinking a lot of alcohol
Symptoms
Signs of bile duct cancer include:
- Yellow skin or eyes (jaundice)
- Pain in your belly or sides
- Upset stomach and vomiting
- Fever
- Loss of appetite or weight loss
- Weakness
- Itching
- Light-colored stools
- Dark urine
Treatment
Its starts with a physical examination. general health, family history of cancer and liver disease, lifestyle, and habits, including drinking and smoking needs to be known. Check for masses, tenderness, or fluid buildup in your belly will also be done.
Certain tests can find signs of bile duct cancer, including:
- Blood tests: It will help to know whether your liver is working the way it should. Others look for signs of tumors, called markers. Need to check your levels of bilirubin, which can cause jaundice when you have a lot of it.
- Abdominal ultrasound: This imaging test helps look for tumors.
- CT scan or MRI: A CT scan is a powerful X-ray that makes detailed pictures inside your body. An MRI uses high-powered magnets to show organs and other things inside your body. If you have a tumor, these can show its size and location, as well as how healthy your liver is.
- Endoscopy: This uses a tool called an endoscope that’s like a camera on the end of a cable. It helps to see inside your body without surgery. They can look at your esophagus, your stomach, and the beginning of your lower intestine.
- Cholangioscopy: This procedure helps check your bile ducts for problems. In ERCP, or endoscopic retrograde cholangiopancreatography, an endoscope is used to inject dye into your bile ducts. They then take X-rays to look for tumors.
- Magnetic resonance cholangiopancreatography (MRCP): This uses an MRI machine to make images of your bile ducts.
- Percutaneous transhepatic cholangiography (PTC): A needle is inserted through your skin and into a bile duct in your liver. It injects dye and takes an X-ray of the area.
- Laparoscopy: Medication is used to put you to sleep and a small cut is made in your belly. A thin tube is inserted with a light and a video camera to look at your bile duct, gallbladder, liver, and other organs and tissues.
- Biopsy: A sample of bile duct cells or tissue is taken, and a technician checks them under a microscope.
You might have one or more of these treatments:
- Biliary drainage: If your bile duct is blocked, a bypass will be required to cut it off and reattach it on the other side of the blockage. A tube called a stent will be put into the duct to keep bile flowing.
- Photodynamic therapy. an inactive form of a certain medication into your vein is injected. The drug tends to collect in more cancer cells than healthy cells. After a few days, an endoscope is used to aim a special light at the tumor. It activates the drug, killing the cancer cells.
- Radiation. This uses high-energy rays or particles to kill cancer cells & to shrink a tumor. After surgery, it can kill any cancer cells that remain. If the cancer can’t be removed but doesn't spread, radiation can help keep it under control.
- Chemotherapy. As with radiation, medicines are often used to kill cancer cells before or after surgery. You can take chemo by mouth or through a shot into a vein.
- Surgery. Depending on the cancer’s spread, it might be needed to remove some or all of your bile duct, lymph nodes, liver, pancreas, or small intestine.
- Liver transplant. This is a rare treatment that can sometimes cure bile duct cancer.
Preventive measures
Even during cancer treatment, you can take steps to feel as healthy as possible. Start by cutting down on alcohol and quitting tobacco.
Cancer often causes fatigue, or extreme tiredness. You might be so tired that it’s hard to do the things you want to do. Rest will help, but so will some exercise.
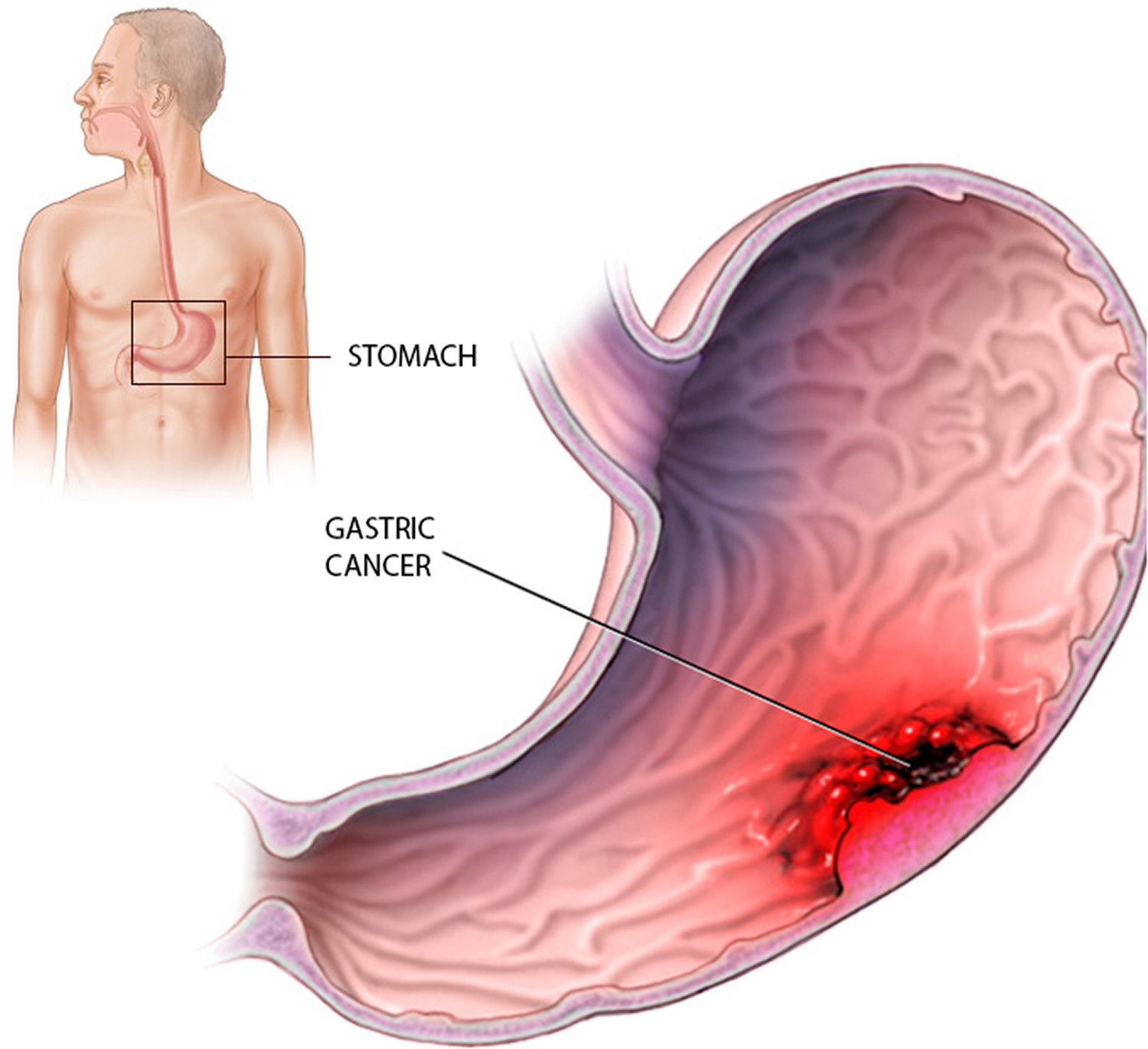
What is Stomach cancer
Stomach cancer begins when cancer cells form in the inner lining of your stomach. These cells can grow into a tumor. Also called gastric cancer, the disease usually grows slowly over many years.
Almost all stomach cancers (about 95%) start in the glandular tissue that lines the stomach. The tumor may spread along the stomach wall or may grow directly through the wall and shed cells into the bloodstream or lymphatic system. Once beyond the stomach, cancer can spread to other organs.
Stomach cancers are classified according to the type of tissue they start in.
- Adenocarcinomas -- the most common -- start in the glandular stomach lining.
- Lymphomas develop from lymphocytes, a type of blood cell involved in the immune system.
- Sarcomas involve the connective tissue (muscle, fat, or blood vessels).
- Other types include carcinoid, small cell carcinoma, and squamous cell carcinoma.
- Metastatic cancers from breast cancer, melanoma, and other primary sites of cancer are also seen in the stomach.
Causes
Infection with a common bacteria, H. pylori, which causes ulcers which raise the risk for the disease. Inflammation in your gut called gastritis, a certain type of long-lasting anemia called pernicious anemia, and growths in your stomach called polyps also can make you more likely to get cancer.
Other things that seem to play a role in raising the risk include:
- Smoking
- Being overweight or obese
- A diet high in smoked, pickled, or salty foods
- Drinking alcohol regularly
- Stomach surgery for an ulcer
- Type-A blood
- Epstein-Barr virus infection
- Certain genes
- Working in coal, metal, timber, or rubber industries
- Exposure to asbestos
- Family history of gastric cancer
- Hereditary factors
Symptoms
Signs and symptoms of stomach cancer may include:
- Difficulty swallowing
- Feeling bloated after eating
- Feeling full after eating small amounts of food
- Heartburn
- Indigestion
- Nausea
- Stomach pain
- Unintentional weight loss
- Vomiting
Treatment
To find out if you have stomach cancer starts with a physical exam. Your medical history is needed to see if you have any risk factors for stomach cancer or any family members who’ve had it. Then, tests which can be:
- Blood tests to look for signs of cancer in your body.
- Upper endoscopy.
- Upper GI series test. You’ll drink a chalky liquid with a substance called barium. The fluid coats your stomach and makes it show up more clearly on X-rays.
- CT scan.This is a powerful X-ray that makes detailed pictures of the inside of your body.
- Biopsy.Your doctor takes a small piece of tissue from your stomach to look at under a microscope for signs of cancer cells. They might do this during an endoscopy.
Your treatment will depend on how long you've had the disease or how much it has spread in your body, called the stage of your cancer:
- Stage 0. This is when the inside lining of your stomach has a group of unhealthy cells that may turn into cancer. Surgery usually cures it. A part or all of your stomach will be removed, as well as nearby lymph nodes -- small organs that are part of your body's germ-fighting system.
- Stage I. At this point, you have a tumor in your
stomach's lining, and it may have spread into your lymph
nodes. As with stage 0, you'll likely have surgery to
remove part or all of your stomach and nearby lymph
nodes. You might also get chemotherapy or
chemoradiation. These treatments can be used before
surgery to shrink the tumor and afterward to kill any
cancer that's left.
Chemotherapy uses drugs to attack cancer cells. Chemoradiation is chemo plus radiation therapy, which destroys cancer cells with beams of high energy. - Stage II. Cancer has spread into deeper layers of the stomach and maybe into nearby lymph nodes. Surgery to remove part or all of your stomach, as well as nearby lymph nodes, is still the main treatment. You're very likely to get chemo or chemoradiation beforehand, and you might get one of them after, too.
- Stage III. The cancer may now be in all layers of the stomach, as well as other organs close by, like the spleen or colon. Or, it may be smaller but reach deep into your lymph nodes. You usually have surgery to remove your entire stomach, along with chemo or chemoradiation.
- Stage IV. In this last stage, cancer has spread far and wide to organs like the liver, lungs, or brain. It's much harder to cure but can be managed to give you some relief from symptoms.
If the tumor blocks part of your GI system, you may get:
- A procedure that destroys part of the tumor with a laser on an endoscope, a thin tube that slides down your throat.
- A thin metal tube called a stent that can keep things flowing. You can get one of these between your stomach and esophagus or between your stomach and small intestine.
- Gastric bypass surgery to create a route around the tumor.
- Surgery to remove part of your stomach.
Chemo, radiation, or both may be used at this stage, too.
Preventive measures
- Treat stomach infections. If you have ulcers from an H. pylori infection, get treatment. Antibiotics can kill the bacteria, and other drugs will heal the sores in the lining of your stomach to cut your risk of cancer.Eat healthy.
- Get more fresh fruits and vegetables on your plate every day. They’re high in fiber and in some vitamins that can lower your cancer risk.
- Avoid very salty, pickled, cured, or smoked foods like hot dogs, processed lunch meats, or smoked cheeses.
- Keep your weight at a healthy level, too. Being overweight or obese can also raise your risk of the disease.
- Don’t smoke. Your stomach cancer risk doubles if you use tobacco