Stomach
Information you need to understand your disease and the tests you may need.
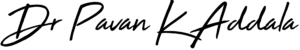
What is liver Acidity/Gastritis
Gastritis is an inflammation, irritation, or erosion of the lining of the stomach. It can occur suddenly (acute) or gradually (chronic).
Causes
Gastritis can be caused by irritation due to excessive alcohol use, chronic vomiting, stress, or the use of certain medications such as aspirin or other anti-inflammatory drugs. It may also be caused by any of the following:
- Helicobacter pylori (H. pylori): A bacteria that lives in the mucous lining of the stomach; without treatment, the infection can lead to ulcers, and in some people, stomach cancer.
- Bile reflux: A backflow of bile into the stomach from the bile tract (that connects to the liver and gallbladder)
- Infections caused by bacteria and viruses
If gastritis is left untreated, it can lead to a severe loss of blood and may increase the risk of developing stomach cancer.
Symptoms
The most common symptoms include:
- Nausea or recurrent upset stomach
- Abdominal bloating
- Abdominal pain
- Vomiting
- Indigestion
- Burning or gnawing feeling in the stomach between meals or at night
- Hiccups
- Loss of appetite
- Vomiting blood or coffee ground-like material
- Black, tarry stools
Treatment
To diagnose gastritis, your personal and family medical history will be reviewed, perform a thorough physical evaluation, and may recommend any of the following tests:
- Upper endoscopy An endoscope, a thin tube containing a tiny camera, is inserted through your mouth and down into your stomach to look at the stomach lining. It is done to check for inflammation and may perform a biopsy, a procedure in which a tiny sample of tissue is removed and then sent to a laboratory for analysis.
- Blood tests Various blood tests will be performed, such as checking your red blood cell count to determine whether you have anemia, which means that you do not have enough red blood cells. H. pylori infection and pernicious anemia with blood tests will also be screened.
- Fecal occult blood test (stool test) This test checks for the presence of blood in your stool, a possible sign of gastritis.
Treatment for gastritis usually involves:
Long-term reflux can cause laryngeal ulcers or granulomas, vocal fold scarring, pneumonia, lung scarring (interstitial lung disease), Barrett’s esophagus (precancerous), and in some cases esophageal or throat cancer.
- Taking antacids and other drugs (such as proton pump inhibitors or H-2 blockers) to reduce stomach acid
- Avoiding hot and spicy foods
- For gastritis caused by H. pylori infection, a regimen of several antibiotics plus an acid blocking drug will be prescribed
- If the gastritis is caused by pernicious anemia, B12 vitamin shots will be given.
- Eliminating irritating foods from your diet such as lactose from dairy or gluten from wheat
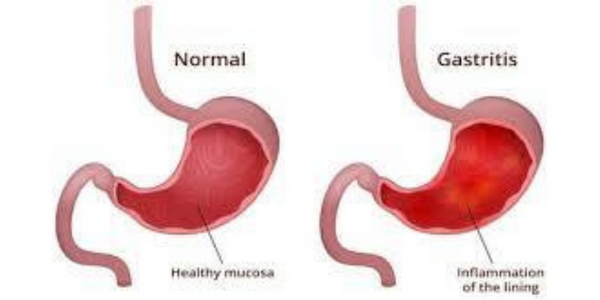
What is Gastric Ulcer
Stomach ulcers, which are also known as gastric ulcers, are painful sores in the stomach lining. Stomach ulcers occur when the thick layer of mucus that protects your stomach from digestive juices is reduced. This allows the digestive acids to eat away at the tissues that line the stomach, causing an ulcer.
Causes
Stomach ulcers are always caused by one of the following:
- an infection with the bacterium Helicobacter pylori (H. pylori)
- long-term use of pain relievers & nonsteroidal anti-inflammatory drugs (NSAIDs), such as aspirin, ibuprofen, or naproxen
- Smoking cigarettes and drinking alcohol also can make you more likely to get ulcers
Symptoms
The most common symptom is a burning sensation or pain in the middle of your abdomen between your chest and belly button. Typically, the pain will be more intense when your stomach is empty, and it can last for a few minutes to several hours.
Other common signs and symptoms of ulcers include:
- dull pain in the stomach
- weight loss
- not wanting to eat because of pain
- nausea or vomiting
- bloating
- feeling easily full
- burping or acid reflux
- heartburn, which is a burning sensation in the chest)
- pain that may improve when you eat, drink, or take antacids
- anemia, whose symptoms can include tiredness, shortness of breath, or paler skin
- dark, tarry stools
- vomit that’s bloody or looks like coffee grounds
Treatment
medical history & bloating in the belly and pain will be checked to make a diagnosis. A series of X-rays or a test called an endoscopy. This test allows a thin, bendy tube to pass down your throat and into your stomach and small intestine. The tube has a camera at the end to check the lining for ulcers. A small piece of the lining can be taken to test for H. pylori. Blood, breath, and stool sample tests also can screen for the bacteria. If your stomach ulcer is the result of H. pylori, you’ll need antibiotics and drugs called proton pump inhibitors (PPIs). PPIs block the stomach cells that produce acid.
In addition to these treatments:
- H2 receptor blockers (drugs that also block acid production)
- stopping use of all NSAIDs
- follow-up endoscopy
- probiotics (useful bacteria that may have a role in killing off H. pylori)
- bismuth supplement
In very rare cases, a complicated stomach ulcer will require surgery. This may be the case for ulcers that:
- continue to return
- don’t heal
- bleed
- tear through the stomach
- keep food from flowing out of the stomach into the small intestine
Surgery may include:
- removal of the entire ulcer
- taking tissue from another part of the intestines and patching it over the ulcer site
- tying off a bleeding artery
- cutting off the nerve supply to the stomach to reduce the production of stomach acid
Preventive measures
Some people who have arthritis or other conditions that cause chronic pain take nonsteroidal anti-inflammatory drugs (NSAIDs) for weeks or months at a time to ease pain and swelling. These medicines can affect the mucus that protects your stomach against acid and make you more likely to have stomach ulcers.
To lower your chances for peptic ulcers while you take NSAIDs:
- Use the lowest possible dose to control your symptoms, and stop taking them as soon as you no longer need them.
- Take your medicine with food.
- Dn't drink alcohol while you’re taking these medicines.
- Don’t smoke, and limit alcohol. These two habits make you more likely to get stomach ulcers. Both thin the mucus lining that protects your stomach from acid, leading to more acid.
- Manage stress. Stress can make the symptoms of a stomach ulcer worse.
- Consider probiotics. Millions of bacteria normally live in your gut. Some, like H. pylori, cause disease. Others are good for you because they help crowd out harmful bacteria. These helpful bacteria are called probiotics.
- Prevent H. pylori infection.You can do some things to make an infection less likely:
- Wash your hands often during the day with warm water and soap so you don't catch or spread H. pylori bacteria
- Cook meat and other foods all the way through
- Only drink water that you know is clean.
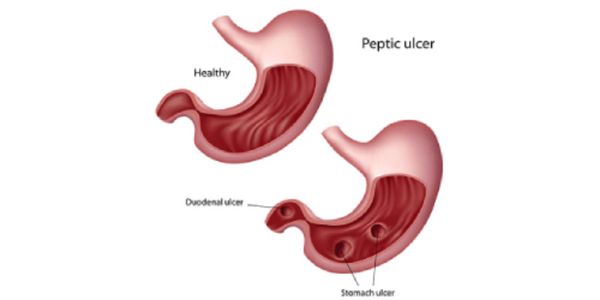
What is Stomach cancer
Stomach cancer begins when cancer cells form in the inner lining of your stomach. These cells can grow into a tumor. Also called gastric cancer, the disease usually grows slowly over many years.
Almost all stomach cancers (about 95%) start in the glandular tissue that lines the stomach. The tumor may spread along the stomach wall or may grow directly through the wall and shed cells into the bloodstream or lymphatic system. Once beyond the stomach, cancer can spread to other organs.
Stomach cancers are classified according to the type of tissue they start in.
- Adenocarcinomas -- the most common -- start in the glandular stomach lining.
- Lymphomas develop from lymphocytes, a type of blood cell involved in the immune system.
- Sarcomas involve the connective tissue (muscle, fat, or blood vessels).
- Other types include carcinoid, small cell carcinoma, and squamous cell carcinoma.
- Metastatic cancers from breast cancer, melanoma, and other primary sites of cancer are also seen in the stomach.
Causes
Infection with a common bacteria, H. pylori, which causes ulcers which raise the risk for the disease. Inflammation in your gut called gastritis, a certain type of long-lasting anemia called pernicious anemia, and growths in your stomach called polyps also can make you more likely to get cancer.
Other things that seem to play a role in raising the risk include:
- Smoking
- Being overweight or obese
- A diet high in smoked, pickled, or salty foods
- Drinking alcohol regularly
- Stomach surgery for an ulcer
- Type-A blood
- Epstein-Barr virus infection
- Certain genes
- Working in coal, metal, timber, or rubber industries
- Exposure to asbestos
- Family history of gastric cancer
- Hereditary factors
Symptoms
Signs and symptoms of stomach cancer may include:
- Difficulty swallowing
- Feeling bloated after eating
- Feeling full after eating small amounts of food
- Heartburn
- Indigestion
- Nausea
- Stomach pain
- Unintentional weight loss
- Vomiting
Treatment
To find out if you have stomach cancer starts with a physical exam. Your medical history is needed to see if you have any risk factors for stomach cancer or any family members who’ve had it. Then, tests which can be:
- Blood tests to look for signs of cancer in your body.
- Upper endoscopy.
- Upper GI series test. You’ll drink a chalky liquid with a substance called barium. The fluid coats your stomach and makes it show up more clearly on X-rays.
- CT scan.This is a powerful X-ray that makes detailed pictures of the inside of your body.
- Biopsy.Your doctor takes a small piece of tissue from your stomach to look at under a microscope for signs of cancer cells. They might do this during an endoscopy.
Your treatment will depend on how long you've had the disease or how much it has spread in your body, called the stage of your cancer:
- Stage 0. This is when the inside lining of your stomach has a group of unhealthy cells that may turn into cancer. Surgery usually cures it. A part or all of your stomach will be removed, as well as nearby lymph nodes -- small organs that are part of your body's germ-fighting system.
- Stage I. At this point, you have a tumor in your stomach's lining, and it may have spread into your lymph nodes. As with stage 0, you'll likely have surgery to remove part or all of your stomach and nearby lymph nodes. You might also get chemotherapy or chemoradiation. These treatments can be used before surgery to shrink the tumor and afterward to kill any cancer that's left.
Chemotherapy uses drugs to attack cancer cells. Chemoradiation is chemo plus radiation therapy, which destroys cancer cells with beams of high energy. - Stage II. Cancer has spread into deeper layers of the stomach and maybe into nearby lymph nodes. Surgery to remove part or all of your stomach, as well as nearby lymph nodes, is still the main treatment. You're very likely to get chemo or chemoradiation beforehand, and you might get one of them after, too.
- Stage III. The cancer may now be in all layers of the stomach, as well as other organs close by, like the spleen or colon. Or, it may be smaller but reach deep into your lymph nodes. You usually have surgery to remove your entire stomach, along with chemo or chemoradiation.
- Stage IV. In this last stage, cancer has spread far and wide to organs like the liver, lungs, or brain. It's much harder to cure but can be managed to give you some relief from symptoms.
If the tumor blocks part of your GI system, you may get:
- A procedure that destroys part of the tumor with a laser on an endoscope, a thin tube that slides down your throat.
- A thin metal tube called a stent that can keep things flowing. You can get one of these between your stomach and esophagus or between your stomach and small intestine.
- Gastric bypass surgery to create a route around the tumor.
- Surgery to remove part of your stomach.
Chemo, radiation, or both may be used at this stage, too.
Preventive measures
- Treat stomach infections. If you have ulcers from an H. pylori infection, get treatment. Antibiotics can kill the bacteria, and other drugs will heal the sores in the lining of your stomach to cut your risk of cancer.Eat healthy.
- Get more fresh fruits and vegetables on your plate every day. They’re high in fiber and in some vitamins that can lower your cancer risk.
- Avoid very salty, pickled, cured, or smoked foods like hot dogs, processed lunch meats, or smoked cheeses.
- Keep your weight at a healthy level, too. Being overweight or obese can also raise your risk of the disease.
- Don’t smoke. Your stomach cancer risk doubles if you use tobacco