Colorectal
Information you need to understand your disease and the tests you may need.
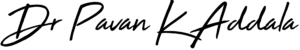
What is piles
Hemorrhoids (HEM-uh-roids), also called piles, are swollen veins in your anus and lower rectum, similar to varicose veins. Hemorrhoids can develop inside the rectum (internal hemorrhoids) or under the skin around the anus (external hemorrhoids).
Causes
The veins around your anus tend to stretch under pressure and may bulge or swell. Piles can develop from increased pressure in the lower rectum due to:
- Straining during bowel movements
- Sitting for long periods of time on the toilet
- Having chronic diarrhea or constipation
- Being obese
- Being pregnant
- Having anal intercourse
- Eating a low-fiber diet
- Regular heavy lifting
Symptoms
Signs and symptoms of hemorrhoids usually depend on the type of hemorrhoid.
External hemorrhoids
These are under the skin around your anus. Signs and symptoms might include:
- Itching or irritation in your anal region
- Pain or discomfort
- Swelling around your anus
- Bleeding
If blood pools in an external hemorrhoid and forms a clot, it can result in:
- Severe pain
- Swelling
- Inflammation
- A hard lump near your anus
Internal hemorrhoids
Internal hemorrhoids lie inside the rectum. You usually can't see or feel them, and they rarely cause discomfort. But straining or irritation when passing stool can cause:
- Painless bleeding during bowel movements. You might notice small amounts of bright red blood on your toilet tissue or in the toilet.
- A hemorrhoid to push through the anal opening (prolapsed or protruding hemorrhoid), resulting in pain and irritation.
We might want to examine your entire colon using colonoscopy if:
- Your signs and symptoms suggest you might have another digestive system disease
- You have risk factors for colorectal cancer
- You are middle-aged and haven't had a recent colonoscopy
Treatment
We might be able to see external hemorrhoids. Diagnosing internal hemorrhoids might include examination of your anal canal and rectum.
- Digital examinationWe insert a gloved, lubricated finger into your rectum. We or she feels for anything unusual, such as growth.
- Visual inspection Because internal hemorrhoids are often too soft to be felt during a rectal exam, we might examine the lower portion of your colon and rectum with an anoscope, proctoscope or sigmoidoscope.
Home remedies
You can often relieve the mild pain, swelling and inflammation of hemorrhoids with home treatments.
- Eat high-fiber foods.
- Use topical treatments.
- Soak regularly in a warm bath
- Take oral pain relievers.
Medications
If your hemorrhoids produce only mild discomfort, your doctor might suggest over-the-counter creams, ointments, suppositories or pads. These products contain ingredients such as witch hazel, or hydrocortisone and lidocaine, which can temporarily relieve pain and itching.
Surgical procedures
Only a small percentage of people with hemorrhoids require surgery
- Hemorrhoid removal (hemorrhoidectomy) : Choosing one of various techniques, your surgeon removes excessive tissue that causes bleeding. The surgery can be done with local anesthesia combined with sedation, spinal anesthesia or general anesthesia. Hemorrhoidectomy is the most effective and complete way to treat severe or recurring hemorrhoids. Complications can include temporary difficulty emptying your bladder, which can result in urinary tract infections. This complication occurs mainly after spinal anesthesia. Most people have some pain after the procedure, which medications can relieve. Soaking in a warm bath also might help.
- Hemorrhoid stapling : This procedure, called stapled hemorrhoidopexy, blocks blood flow to hemorrhoidal tissue. It is typically used only for internal hemorrhoids. Stapling generally involves less pain than hemorrhoidectomy and allows for earlier return to regular activities. Compared with hemorrhoidectomy, however, stapling has been associated with a greater risk of recurrence and rectal prolapse, in which part of the rectum protrudes from the anus. Complications can also include bleeding, urinary retention and pain, as well as, rarely, a life-threatening blood infection (sepsis). Talk with your doctor about the best option for you.
- External hemorrhoid thrombectomy : If a painful blood clot (thrombosis) has formed within an external hemorrhoid, your doctor can remove the hemorrhoid, which can provide prompt relief. This procedure, done under local anesthesia, is most effective if done within 72 hours of developing a clot.
- Rubber band ligation : Your doctor places one or two tiny rubber bands around the base of an internal hemorrhoid to cut off its circulation. The hemorrhoid withers and falls off within a week. Hemorrhoid banding can be uncomfortable and cause bleeding, which might begin two to four days after the procedure but is rarely severe. Occasionally, more-serious complications can occur.
- Injection (sclerotherapy) : Your doctor injects a chemical solution into the hemorrhoid tissue to shrink it. While the injection causes little or no pain, it might be less effective than rubber band ligation.
- Coagulation (infrared, laser or bipolar) : Coagulation techniques use laser or infrared light or heat. They cause small, bleeding internal hemorrhoids to harden and shrivel. Coagulation has few side effects and usually causes little discomfort.
Preventive measures
The best way to prevent hemorrhoids is to keep your stools soft, so they pass easily. To prevent hemorrhoids and reduce symptoms of hemorrhoids, follow these tips:
- Eat high-fiber foods.
- Drink plenty of fluids.
- Consider fiber supplements.
- Don't strain.
- Go as soon as you feel the urge.
- Exercise.
- Avoid long periods of sitting.
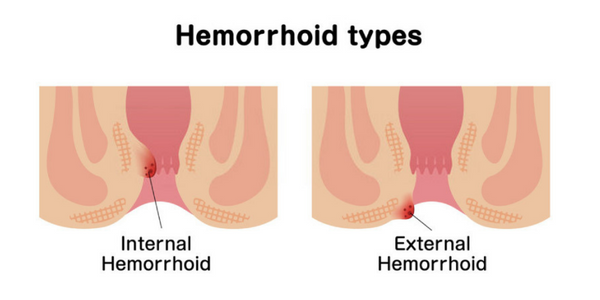
What is fissures
An anal fissure is a cut or a tear in the thin, delicate lining of your anus. The tear often exposes the muscle around the anus, called the anal sphincter. The damage can cause that muscle to spasm, which can pull apart the edges of the fissure even more. The spasms can cause pain and slow down the healing. Bowel movements can also keep the fissures from getting better.
Causes
Causes of anal fissure include:
- Passing large or hard
- Constipation and straining during bowel movements
- Chronic diarrhea
- Childbirth
- Crohn's disease or another inflammatory bowel disease
- Anal cancer
- HIV
- Tuberculosis
- Syphilis
Symptoms
Signs and symptoms of an anal fissure include:
- Pain, sometimes severe, during bowel movements
- Pain after bowel movements that can last up to several hours
- Bright red blood on the stool or toilet paper after a bowel movement
- A visible crack in the skin around the anus
- A small lump or skin tag on the skin near the anal fissure
Treatment
A physical exam, including a gentle inspection of the anal region is all that's needed to diagnose an anal fissure. A fissure that occurs on the side of the anal opening, rather than the back or front, is more likely to be a sign of another disorder, such as Crohn's disease. Further testing to analyze the condition would be required:
Anoscopy: An anoscope is a tubular device inserted into the anus to help your doctor visualize the rectum and anus.
Surgical methods: Your doctor will insert a thin, flexible tube with a tiny video into the bottom portion of your colon.
Colonoscopy : Your doctor will insert a flexible tube into your rectum to inspect the entire colon.
Anal fissures often heal within a few weeks if you take steps to keep your stool soft, such as increasing your intake of fiber and fluids.
Nonsurgical treatments
Externally applied nitroglycerin (Rectiv), to help increase blood flow to the fissure and promote healing and to help relax the anal sphincter.
Topical anesthetic creams , such as lidocaine hydrochloride (Xylocaine) may be helpful for pain relief.
Botulinum toxin type A (Botox) injection , to paralyze the anal sphincter muscle and relax spasms.
Blood pressure medications , such as oral nifedipine (Procardia) or diltiazem (Cardizem) can help relax the anal sphincter.
Surgery
If you have a chronic anal fissure that is resistant to other treatments, or if your symptoms are severe, lateral internal sphincterotomy (LIS) can be done, which involves cutting a small portion of the anal sphincter muscle to reduce spasm and pain, and promote healing.
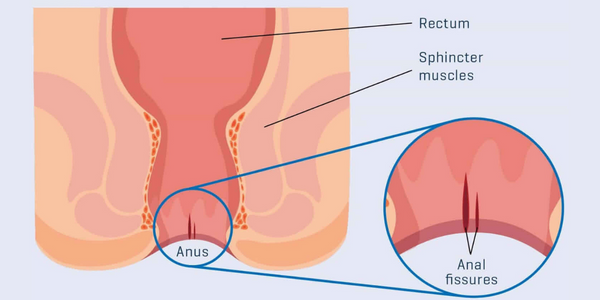
What is anal fistula
An anal fistula is a tunnel that runs from inside the anus -- the hole your body uses to get rid of solid waste -- to somewhere in the skin around it. It usually follows an infection that didn’t heal the right way. Surgery is usually needed to treat anal fistula.
Causes
Just inside your anus are several glands that make fluid. Sometimes, they get blocked or clogged. When that happens, a bacteria buildup can create a swollen pocket of infected tissue and liquid which is called an abscess.If you don’t treat the abscess, it’ll grow.
Eventually, it’ll make its way to the outside and punch a hole in the skin somewhere near your anus so the gunk inside it can drain. The fistula is the tunnel that connects the gland to that opening. Most of the time, an abscess causes a fistula. It’s rare, but they can also come from conditions like tuberculosis, sexually transmitted diseases, or an ongoing illness that affects your bowels, such as Crohn’s disease or ulcerative colitis.
Symptoms
The most common symptoms are:
- Pain
- Redness
- Swelling around your anus
- Bleeding
- Painful bowel movements or urination
- Fever
- A foul-smelling liquid oozing from a hole near your anus
Early esophageal cancer typically causes no signs or symptoms.
Treatment
The doctor will probably send you to a specialist in colon and rectal problems for more exams or imaging tests like X-rays or a CT scan. You might even need a colonoscopy.There’s no medication to fix the condition, so surgery is used. The procedure can usually take place in a doctor’s office or clinic. You won’t have to go to the hospital.
- For a simple fistula that isn’t too close to your anus, the doctor will cut open the skin and muscle surrounding the tunnel. This allows the opening to heal from the inside out.
- They may use a plug to close the fistula.
- For a more complicated fistula, the doctor might put a tube -- known as a seton -- into the opening. This helps drain the infected fluid before surgery. It could take 6 weeks or more.
Depending on where the fistula is, your doctor may have to cut into the sphincter muscles that open and close your anus.
What is anal colorectal cancer
Colon cancer is a type of cancer that begins in the large intestine (colon). The colon is the final part of the digestive tract. Colon cancer typically affects older adults, though it can happen at any age. It usually begins as small, noncancerous (benign) clumps of cells called polyps that form on the inside of the colon. Over time some of these polyps can become colon cancers. If colon cancer develops, many treatments are available to help control it, including surgery, radiation therapy and drug treatments, such as chemotherapy, targeted therapy and immunotherapy.
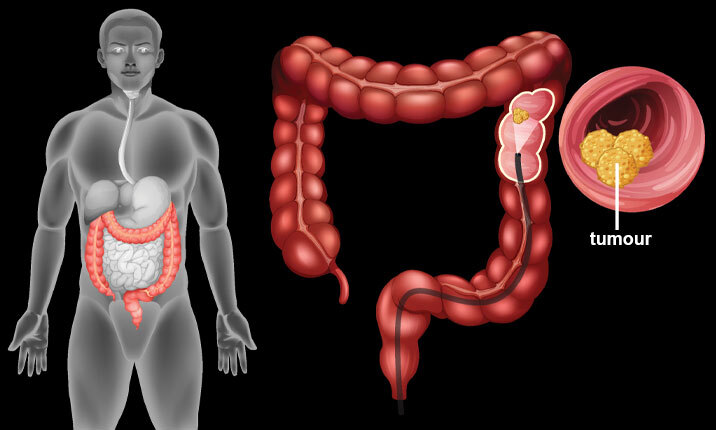
Causes
In general, colon cancer begins when healthy cells in the colon develop changes (mutations) in their DNA. A cell's DNA contains a set of instructions that tell a cell what to do. Healthy cells grow and divide in an orderly way to keep your body functioning normally. But when a cell's DNA is damaged and becomes cancerous, cells continue to divide — even when new cells aren't needed. As the cells accumulate, they form a tumor. With time, the cancer cells can grow to invade and destroy normal tissue nearby. And cancerous cells can travel to other parts of the body to form deposits there (metastasis)
There are several types of colorectal cancer, based on where it starts
- Adenocarcinoma. This is the most common kind, making up 96% of cases. It starts in cells that make mucus for your colon and rectum.
- Carcinoid tumor. This begins in cells that make hormones.
- Gastrointestinal stromal tumor. This forms in cells in the wall of your colon that tell your gastrointestinal muscles to move food or liquid along.
- Lymphoma. This is cancer of your immune system cells.
- Sarcoma. This starts in connective tissues like blood vessels or muscle layers.
Nearly all colon and rectal cancers begin as a polyp, a growth on the inner surface of your colon. Polyps themselves usually aren’t cancer.
- Hyperplastic and inflammatory polyps. These usually don’t carry a chance of cancer. But large hyperplastic polyps, especially on the right side of your colon, can be a problem. Your doctor will want to remove them.
- Adenomas or adenomatous polyps. These are precancerous. If you leave them alone, they could turn into colon cancer
Symptoms
Signs and symptoms of colon cancer include:
- A persistent change in your bowel habits, including diarrhea or constipation or a change in the consistency of your stool
- Rectal bleeding or blood in your stool
- Persistent abdominal discomfort, such as cramps, gas or pain
- A feeling that your bowel doesn't empty completely
- Weakness or fatigue
- Unexplained weight loss
Colorectal Cancer Diagnosis
- Rectal exam. Your doctor can use their fingers to feel for growths.
- Colonoscopy. This is the standard screening test that experts recommend. Your doctor uses a thin, flexible tube called a colonoscope to look at your entire colon and rectum.
- Sigmoidoscopy. Your doctor looks at your rectum and the last part of your colon.
- Biopsy. Your doctor may take out a bit of tissue during a colonoscopy or sigmoidoscopy and send it to a lab for testing. They can also use a needle to take a sample, with a CT scan or ultrasound to guide them. Complications are rare, but you may have some bleeding or discomfort.
- Stool DNA. This test looks for certain gene changes that might be a sign of colon cancer.
- CT colonography. This is a special X-ray (also called a virtual colonoscopy) of your entire colon. It takes less time and is less invasive than other tests. But if it shows a polyp, you’ll still need a colonoscopy.
- Barium enema X-ray. This is a type of X-ray that involves putting dye in your colon. It can find trouble spots that might mean you need a colonoscopy.
- Other imaging tests. MRI or ultrasound can give your doctor a better look at your organs.
Treatment
Which treatments are most likely to help you depends on your particular situation, including the location of your cancer, its stage and your other health concerns.
Surgery for early-stage colon cancer
- polyps during a colonoscopy (polypectomy) If your cancer is small, localized, completely contained within a polyp and in a very early stage, your doctor may be able to remove it completely during a colonoscopy.
- Endoscopic mucosal resection Larger polyps might be removed during colonoscopy using special tools to remove the polyp and a small amount of the inner lining of the colon in a procedure called an endoscopic mucosal resection.
- Minimally invasive surgery (laparoscopic surgery) Polyps that can't be removed during a colonoscopy may be removed using laparoscopic surgery. In this procedure, your surgeon performs the operation through several small incisions in your abdominal wall, inserting instruments with attached cameras that display your colon on a video monitor.
Surgery for more advanced colon cancer
- Partial colectomy During this procedure, the surgeon removes the part of your colon that contains the cancer, along with a margin of normal tissue on either side of the cancer. This procedure can commonly be done by a minimally invasive approach (laparoscopy).
- Surgery to create a way for waste to leave your body When it's not possible to reconnect the healthy portions of your colon or rectum, you may need an ostomy. This involves creating an opening in the wall of your abdomen from a portion of the remaining bowel for the elimination of stool into a bag that fits securely over the opening.
- Lymph node removal Nearby lymph nodes are usually also removed during colon cancer surgery and tested for cancer.
Surgery for advanced cancer
If your cancer is very advanced or your overall health very poor, we may recommend an operation to relieve a blockage of your colon or other conditions in order to improve your symptoms.
Chemotherapy
Chemotherapy uses drugs to destroy cancer cells. Chemotherapy for colon cancer is usually given after surgery if the cancer is larger or has spread to the lymph nodes. In this way, chemotherapy may kill any cancer cells that remain in the body and help reduce the risk of cancer recurrence
Chemotherapy might also be used before an operation to shrink a large cancer so that it's easier to remove with surgery
Chemotherapy can also be used to relieve symptoms of colon cancer that can't be removed with surgery or that has spread to other areas of the body. Sometimes it's combined with radiation therapy.
Radiation therapy
Radiation therapy uses powerful energy sources, such as X-rays and protons, to kill cancer cells. It might be used to shrink a large cancer before an operation so that it can be removed more easily. When surgery isn't an option, radiation therapy might be used to relieve symptoms, such as pain.
Targeted drug therapy
Targeted drug treatments focus on specific abnormalities present within cancer cells. By blocking these abnormalities, targeted drug treatments can cause cancer cells to die. Targeted drugs are usually combined with chemotherapy.
Immunotherapy
Immunotherapy is a drug treatment that uses your immune system to fight cancer. Your body's disease-fighting immune system may not attack your cancer because the cancer cells produce proteins that blind the immune system cells from recognizing the cancer cells. Immunotherapy works by interfering with that process.
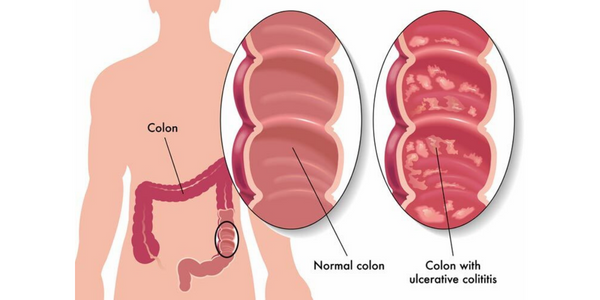
What is ulcerative colitis
Doctors often classify ulcerative colitis according to its location. Types of ulcerative colitis include:
- Ulcerative proctitis Inflammation is confined to the area closest to the anus (rectum), and rectal bleeding may be the only sign of the disease.
- Proctosigmoiditis Inflammation involves the rectum and sigmoid colon — the lower end of the colon. Signs and symptoms include bloody diarrhea, abdominal cramps and pain, and an inability to move the bowels in spite of the urge to do so (tenesmus).
- Left-sided colitis Inflammation extends from the rectum up through the sigmoid and descending colon. Signs and symptoms include bloody diarrhea, abdominal cramping and pain on the left side, and urgency to defecate.
- Pancolitis This type often affects the entire colon and causes bouts of bloody diarrhea that may be severe, abdominal cramps and pain, fatigue, and significant weight loss.
Causes
One possible cause is an immune system malfunction. When your immune system tries to fight off an invading virus or bacterium, an abnormal immune response causes the immune system to attack the cells in the digestive tract, too. Heredity also seems to play a role in that ulcerative colitis is more common in people who have family members with the disease. However, most people with ulcerative colitis don't have this family history.
Possible complications of ulcerative colitis include:
- Severe bleeding
- A hole in the colon (perforated colon)
- Severe dehydration
- Bone loss (osteoporosis)
- Inflammation of your skin, joints and eyes
- An increased risk of colon cancer
- A rapidly swelling colon (toxic megacolon)
- Increased risk of blood clots in veins and arteries
Symptoms
Ulcerative colitis symptoms can vary, depending on the severity of inflammation and where it occurs. Signs and symptoms may include:
- Diarrhea, often with blood or pus
- Abdominal pain and cramping
- Rectal pain
- Rectal bleeding — passing small amount of blood with stool
- Urgency to defecate
- Inability to defecate despite urgency
- Weight loss
- Fatigue
- Fever
- In children, failure to grow
Treatment
UC treatment has two main goals. The first is to make you feel better and give your colon a chance to heal. The second is to prevent more flare-ups. You may need a combination of diet changes, medication, or surgery to reach those goals. Diet. Some foods can make your symptoms worse. You might find that soft, bland food doesn’t bother you as much as spicy or high-fiber dishes. If you can’t digest the sugar in milk called lactose (meaning you’re lactose intolerant), your doctor may tell you to stop eating dairy products. A balanced diet with plenty of fiber, lean protein, fruits, and veggies should provide enough vitamins and nutrients.
Medicine
- Antibiotics These fight infections and let your large intestine heal.
- Aminosalicylates These drugs have something called 5-aminosalicylic acid (5-ASA) that fights inflammation and helps control symptoms. You might get pills to swallow or an enema or suppository to put in your bottom.
- Corticosteroids If aminosalicylates don’t work or your symptoms are severe, your doctor might give you these anti-inflammatory drugs for a short time.
- Immunomodulators These help stop your immune system’s attack on your colon. They can take a while to take effect. You might not notice any changes for up to 3 months.
- Biologics These are made from proteins in living cells instead of chemicals. They’re for people with severe ulcerative colitis.
- Janus kinase inhibitors (JAK inhibitors) These are oral medicines that can work quickly to get and maintain a remission in ulcerative colitis.
- Sphingosine 1-phosphate (S1P) receptor modulators This is an oral medication for patients with moderately to severely active UC.
- Loperamide This can slow or stop diarrhea Talk to your doctor before taking it.
Surgery. If other treatments don’t work or your UC is severe, you might need surgery to remove your colon (colectomy) or colon and rectum (proctocolectomy). If you have a proctocolectomy, we will have to make a small pouch out of your small intestine and attach it to your anus. It lets your body expel waste normally, so you don’t need to wear a bag to collect stool.
Preventive measures
Sometimes you may feel helpless when facing ulcerative colitis. But changes in your diet and lifestyle may help control your symptoms and lengthen the time between flare-ups.
There's no firm evidence that what you eat actually causes inflammatory bowel disease. But certain foods and beverages can aggravate your signs and symptoms, especially during a flare-up.
It can be helpful to keep a food diary to keep track of what you're eating, as well as how you feel. If you discover that some foods are causing your symptoms to flare, you can try eliminating them.
- Limit dairy products You may be lactose intolerant — that is, your body can't digest the milk sugar (lactose) in dairy foods.
- Eat small meals You may find that you feel better eating five or six small meals a day rather than two or three larger ones.
- Drink plenty of liquids Try to drink plenty of liquids daily. Water is best. Alcohol and beverages that contain caffeine stimulate your intestines and can make diarrhea worse, while carbonated drinks frequently produce gas.
- Talk to a dietitian If you begin to lose weight or your diet has become very limited, talk to a registered dietitian.
- Exercise Even mild exercise can help reduce stress, relieve depression and normalize bowel function.
- Biofeedback This stress-reduction technique helps you reduce muscle tension and slow your heart rate with the help of a feedback machine.
- Regular relaxation and breathing exercises An effective way to cope with stress is to perform relaxation and breathing exercises.
What is anal diverticulitis
Diverticula are small, bulging pouches that can form in the lining of your digestive system. They are found most often in the lower part of the large intestine (colon).
The presence of diverticula is known as diverticulosis. When one or more of the pouches become inflamed, and in some cases infected, that condition is known as diverticulitis. Diverticulitis can cause severe abdominal pain, fever, nausea and a marked change in your bowel habits. Mild diverticulitis can be treated with rest, changes in your diet and antibiotics. Severe or recurring diverticulitis may require surgery.
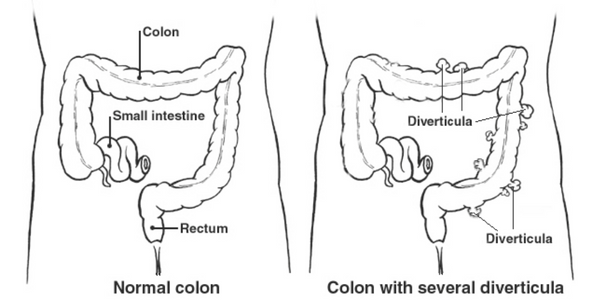
Causes
Diverticula usually develop when naturally weak places in your colon give way under pressure. This causes marble-sized pouches to protrude through the colon wall.Diverticulitis occurs when diverticula tear, resulting in inflammation, and in some cases, infection.
Several factors may increase your risk of developing diverticulitis:
- Aging The incidence of diverticulitis increases with age.
- Obesity Being seriously overweight increases your odds of developing diverticulitis.
- Smoking People who smoke cigarettes are more likely than nonsmokers to experience diverticulitis.
- Lack of exercis Vigorous exercise appears to lower your risk of diverticulitis.
- Diet high in animal fat and low in fiber A low-fiber diet in combination with a high intake of animal fat seems to increase risk, although the role of low fiber alone isn't clear.
- Certain medications Several drugs are associated with an increased risk of diverticulitis, including steroids, opioids and nonsteroidal anti-inflammatory drugs
Symptoms
The signs and symptoms of diverticulitis include:
- Pain, which may be constant and persist for several days. The lower left side of the abdomen is the usual site of the pain. Sometimes, however, the right side of the abdomen is more painful.
- Nausea and vomiting.
- Fever.
- Abdominal tenderness.
- Constipation or, less commonly, diarrhea.
If you don’t treat it, diverticulitis can lead to serious complications that require surgery:
- Abscesses, collections of pus from the infection, may form around the infected diverticula. If these go through the intestinal wall, you could get peritonitis. This infection can be fatal.
- Perforation or tearing in the intestinal wall can lead to abscesses and infection because of waste leaking into the abdominal cavity.
- Scarring can lead to a stricture or blockage of the intestine.
- Fistulas can develop if an infected diverticulum reaches a nearby organ and forms a connection. This most often happens between the large intestine and the bladder. It can lead to a kidney infection. Fistulas can also form between the large intestine and either the skin or the vagina.
- Stricture, which happens when the colon narrows in the affected area.
Treatment
The symptoms of diverticulitis can also look like other problems. We will need to narrow things down by ruling out other issues. Post physical examination, the following tests are likely to be suggested.
- Blood and urine tests, to check for signs of infection.
- A pregnancy test for women of childbearing age, to rule out pregnancy as a cause of abdominal pain.
- A liver enzyme test, to rule out liver-related causes of abdominal pain.
- A stool test, to rule out infection in people who have diarrhea.
- A CT scan, which can identify inflamed or infected pouches and confirm a diagnosis of diverticulitis. CT can also indicate the severity of diverticulitis and guide treatment.
Treatment depends on the severity of your signs and symptoms.
Complicated diverticulitis
If you have a severe attack or have other health problems, you'll likely need to be hospitalized. Treatment generally involves:
- Intravenous antibiotics
- Insertion of a tube to drain an abdominal abscess, if one has formed
Surgery
You'll likely need surgery to treat diverticulitis if:
- You have a complication, such as a bowel abscess, fistula or obstruction, or a puncture (perforation) in the bowel wall
- You have had multiple episodes of uncomplicated diverticulitis
- You have a weakened immune system
There are two main types of surgery:
- Primary bowel resection The diseased segments of your intestine are removed and then reconnected with the healthy segments (anastomosis). This allows you to have normal bowel movements. Depending on the amount of inflammation, you may have open surgery or a minimally invasive (laparoscopic) procedure.
- Bowel resection with colostom If you have so much inflammation that it's not possible to rejoin your colon and rectum, colostomy will be performed. An opening (stoma) in your abdominal wall is connected to the healthy part of your colon. Waste passes through the opening into a bag. Once the inflammation has eased, the colostomy may be reversed and the bowel reconnected.
Preventive measures
To help prevent diverticulitis:
- regularly Exercise promotes normal bowel function and reduces pressure inside your colon.
- Eat more fiber A high-fiber diet decreases the risk of diverticulitis. Fiber-rich foods, such as fresh fruits and vegetables and whole grains, soften waste material and help it pass more quickly through your colon.
- Drink plenty of fluids Fiber works by absorbing water and increasing the soft, bulky waste in your colon.
- Avoid smoking Smoking is associated with an increased risk of diverticulitis.
What is volvulus
A volvulus occurs when part of the colon or intestine twists. The twisting causes bowel obstructions that may cut off the blood supply to areas of the bowels. A volvulus is a medical emergency that needs surgical treatment. If left untreated, the parts of the bowels that are not receiving enough blood will start to die.
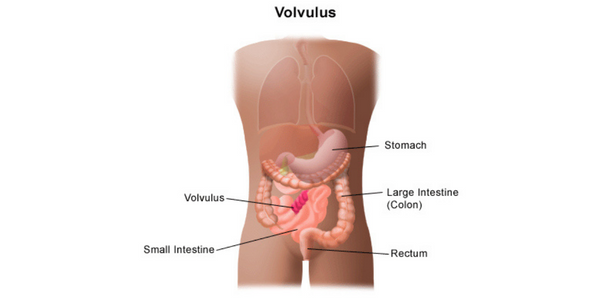
Causes
Volvulus usually occurs due to another underlying condition or physical problem. However, it can sometimes occur on its own. In infants, volvulus of the small intestine often occurs due to malrotation. Malrotation occurs when a problem with the way the intestines form causes them to settle in the wrong place in the abdomen. This can cause the intestines to twist or become blocked.In adults, causes of a volvulus include:
- an enlarged colon
- abdominal adhesions that develop after surgery, injury, or infection
- diseases of the large intestine, such as Hirschsprung’s disease
- a colon that is not attached to the abdominal wall
- a narrow connection at the base of the colon
- chronic constipation
- pregnancy
Symptoms
The symptoms of volvulus appear suddenly and severely, so people usually go straight to the emergency room for prompt evaluation.
Symptoms of volvulus include the following:
- abdominal pain and tenderness
- vomiting green bile
- Nausea
- distended abdomen
- bloody stool
- constipation
- shock
Treatment
If a person shows signs of having a volvulus, a physical examination will be done along with the need of medical history. A few tests will also be required
- blood tests
- tests to examine stool for blood
- barium X-rays for the upper or lower abdominal tract
- computed tomography (CT) scans to check the abdomen for abnormalities
- flexible sigmoidoscopy
A volvulus needs prompt treatment and usually requires surgery. During surgery to correct a volvulus, a small incision is made in the abdominal wall near the site of the twisted part of the intestine and untwist it.
Afterward, the blood flow is restored to the areas affected by the volvulus. If parts of the intestine have been without blood for too long and a portion of the intestine has died, that piece of the intestine will be removed.
Sometimes, so much of the intestine needs to be removed that it is impossible to reattach the ends to each other. If this happens, the two ends of the intestines will be connected to the openings in the abdominal wall known as stomas.
If a person requires a stoma, stool will pass through these openings into a colostomy bag. This may be permanent or temporary.
Sometimes, this procedure leaves a person’s appendix in a different location. If this happens, the appendix is removed.
What is anal rectal prolapse
Prolapse is when any body part slips or falls down from its normal position. Rectal prolapse occurs when part of the large intestine's lowest section (rectum) slips outside the muscular opening at the end of the digestive tract (anus). While rectal prolapse may cause discomfort, it's rarely a medical emergency.
Rectal prolapse can sometimes be treated with stool softeners, suppositories and other medications. But surgery is usually needed to treat rectal prolapse.
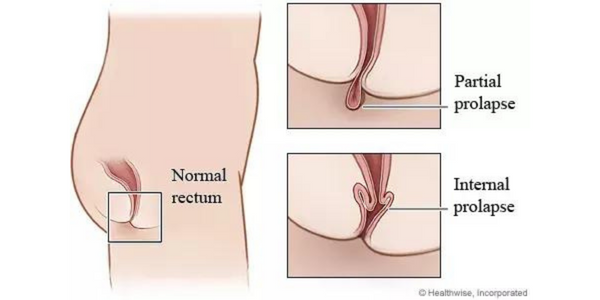
There are three types of prolapse:
- External prolapse: The entire rectum sticks out of your anus.
- prolapse: Part of the rectal lining pokes out of your anus.
- Internal prolapse: The rectum has started to drop but is not yet sticking out of your anus
Causes
A variety of things can cause the condition, including:
- Long-term history of diarrhea or constipation
- Long-term history of having to strain when you poop
- Old age, which weakens muscles and ligaments in the rectal area
- Previous injury to the anal or hip area
- Nerve damage that affects your muscles’ ability to tighten and loosen, which could be caused by pregnancy, vaginal childbirth complications, anal sphincter paralysis, or injury to your spine or back
- Neurological problems, such as spinal cord disease or spinal cord transection
Symptoms
If you feel like you’re sitting on a ball after pooping, or if you notice that you have something sticking out of the opening (your anus) where you poop, you could have rectal prolapse. Additional symptoms of rectal prolapse can include:
- Feeling a bulge outside your anus
- Seeing a red mass outside your anal opening
- Pain in the anus or rectum
- Bleeding from the rectum
- Leaking blood, poop, or mucus from the anus
Treatment
Rectal Prolapse Diagnosis
A rectal examination will be done.You may need some other, more advanced tests to diagnose rectal prolapse, especially if you have other related conditions:
- Anal electromyography (EMG):This test checks to see if nerve damage is causing your anal sphincter problems.Anal manometry: A thin tube is inserted into your rectum to test muscle strength.
- Anal ultrasound: A probe inserted into your anus and rectum is used to examine muscles and tissues.
- Pudendal nerve terminal motor latency test: It checks your pudendal nerves, which you use to control bowel movements.
- Proctography:X-ray videos of your rectum during a poop show how well it holds and releases feces.
- Colonoscopy: A long tube inserted into your rectum with a tiny camera at the end can show the inside of your intestines and look for any problems that may be causing your prolapse.
- Proctosigmoidoscopy:This test also uses a long tube with a camera on the end. It’s inserted deep into your intestines to look for inflammation, scarring, or a tumor.
- MRI: Imaging scan examines all of the organs in your pelvic area.
Preventive measures
To prevent rectal prolapse, try not to strain when you poop. Try these tips to ease or prevent constipation that leads to straining:
- Get more fiber in your diet. Aim for at least five servings of fruits and veggies each day.
- Drink 6 to 8 glasses of water a day.
- Get regular exercise.
- Keep your weight at a healthy level or lose weight if you need to.
- If you have constipation often, talk to your doctor. They may direct you to take a stool softener or laxative.
- Avoid heavy lifting, as this could put pressure on your bowel muscles.