Pancreas
Information you need to understand your disease and the tests you may need.
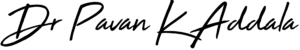
What is pancreatitis
The pancreas is a large gland behind your stomach and next to your small intestine. Your pancreas does two main things:
- It releases powerful digestive enzymes into your small intestine to help you digest food.
- It releases insulin and glucagon into your bloodstream. These hormones help your body control how it uses food for energy.
Your pancreas can be damaged when digestive enzymes begin working before your pancreas releases them. Pancreatitis can occur as acute pancreatitis — meaning it appears suddenly and lasts for days. Some people develop chronic pancreatitis, which is pancreatitis that occurs over many years.
Causes
With repeated bouts of acute pancreatitis, damage to the pancreas can occur and lead to chronic pancreatitis.
- Gallstones
- Alcoholism
- Certain medications
- High triglyceride levels in the blood (hypertriglyceridemia)
- High calcium levels in the blood (hypercalcemia), which may be caused by an overactive parathyroid gland (hyperparathyroidism)
- Pancreatic cancer
- Abdominal surgery
- Cystic fibrosis
- Infection
- Injury to the abdomen
- Obesity
- Trauma
Symptoms
The two forms of pancreatitis are acute and chronic.
- Acute pancreatitis is sudden inflammation that lasts a short time. It can range from mild discomfort to a severe, life-threatening illness. In severe cases, acute pancreatitis can cause bleeding, serious tissue damage, infection, and cysts. Severe pancreatitis can also harm other vital organs such as the heart, lungs, and kidneys.
- Chronic pancreatitis is long-lasting inflammation. It most often happens after an episode of acute pancreatitis. Another top cause is drinking lots of alcohol for a long period of time. Damage to your pancreas from heavy alcohol use may not cause symptoms for many years, but then you may suddenly have severe pancreatitis symptoms.
Pancreatitis can have severe complications, including:
- Diabetes if there’s damage to the cells that produce insulin
- Infection of your pancreas
- Kidney failure
- Malnutrition if your body can’t get enough nutrients from the food you eat because of a lack of digestive enzymes
- Pancreatic cancer
- Pancreatic necrosis, when tissues die because your pancreas isn’t getting enough blood
- Problems with your breathing when chemical changes in your body affect your lungs
- Pseudocysts, when fluid collects in pockets on your pancreas. They can burst and become infected.
Treatment
To diagnose chronic pancreatitis, X-rays or imaging tests such as a CT scan or MRI may show whether the pancreas is calcified. Blood samples and check your stool for excess fat, a sign that the pancreas is no longer making enough enzymes to process fat. You may be given a pancreatic function test to see how well the pancreas releases digestive enzymes. You may also be checked for diabetes.
To diagnose acute pancreatitis, your blood will be tested to measure two digestive enzymes: amylase and lipase. High levels of these two enzymes mean you probably have acute pancreatitis. They’ll also test your blood for white blood cells, blood sugar, calcium, and liver function.
Other tests can include:
- Pancreatic function test to find out whether your pancreas is making the right amounts of digestive enzymes
- Ultrasound, CT scan, and MRI, which make images of your pancreas to show the extent of inflammation, causes such as bile duct problems and gallstones, for complications like cysts.
- ERCP, a long tube with a camera on the end to look at your pancreatic and bile ducts is inserted.
- Biopsy, in which a needle is used to remove a small piece of tissue from your pancreas to be studied
Your blood and poop may be tested to confirm the diagnosis. A glucose tolerance test can be done to measure damage to the cells in your pancreas that make insulin.
How Is Pancreatitis Treated?
If you have an attack of acute pancreatitis, you may receive strong drugs for pain. You may have to have your stomach drained with a tube placed through your nose. If the attack is prolonged, you may be fed and hydrated intravenously (through a vein). You’ll probably need to stay in the hospital, where your treatment may include:
- Antibiotics if your pancreas is infected
- Intravenous (IV) fluids, given through a needle
- Low-fat diet or fasting. You might need to stop eating so your pancreas can recover. In this case, you’ll get nutrition through a feeding tube.
- Pain medicine
If your case is more severe, your treatment might include:
- Endoscopic retrograde cholangiopancreatography (ERCP), a procedure that involves the insertion of a tube down your throat into the stomach and upper intestines to take out gallstones if they’re blocking your bile or pancreatic ducts. A small cut is made to remove stones in the bile duct, or a plastic tube called a stent is inserted into the ducts to relieve the obstruction.
- Gallbladder surgery if gallstones caused your pancreatitis
- Pancreas surgery to clean out fluid or dead or diseased tissue
Treatment for chronic pancreatitis
If you have chronic pancreatitis, treating pain -- guarding against possible addiction to prescription painkillers -- and watching for complications that affect digestion will be suggested. You may be placed on a pancreatic enzyme replacement therapy to restore the digestive tract's ability to digest nutrients; this will also likely reduce the frequency of new attacks.
You might need:
- Insulin to treat diabetes
- Pain medicine
- Pancreatic enzymes to help your body get enough nutrients from your food
- Surgery or procedures to relieve pain, help with drainage, or treat blockages
Injection of anesthetics into the nerves near the spine may give pain relief. If the pain does not respond to medication or nerve blocks, the damaged pancreatic tissue may be surgically removed, but only as a last resort.
Preventive measures
- Stop drinking alcohol
- Stop smoking
- Choose a low-fat diet
- Drink more fluids
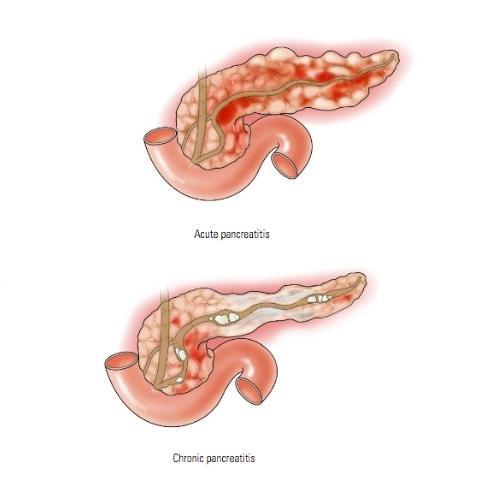
What is Pancreatic Cancer
Pancreatic cancer begins in the tissues of your pancreas — an organ in your abdomen that lies behind the lower part of your stomach. Your pancreas releases enzymes that aid digestion and produces hormones that help manage your blood sugar.
Several types of growths can occur in the pancreas, including cancerous and noncancerous tumors. The most common type of cancer that forms in the pancreas begins in the cells that line the ducts that carry digestive enzymes out of the pancreas (pancreatic ductal adenocarcinoma).
Pancreatic cancer treatment options are chosen based on the extent of the cancer. Options may include surgery, chemotherapy, radiation therapy or a combination of these.
Causes
Pancreatic cancer occurs when cells in your pancreas develop changes (mutations) in their DNA. A cell's DNA contains the instructions that tell a cell what to do. These mutations tell the cells to grow uncontrollably and to continue living after normal cells would die. These accumulating cells can form a tumor. When left untreated, the pancreatic cancer cells can spread to nearby organs and blood vessels and to distant parts of the body.
Most pancreatic cancer begins in the cells that line the ducts of the pancreas. This type of cancer is called pancreatic adenocarcinoma or pancreatic exocrine cancer. Less frequently, cancer can form in the hormone-producing cells or the neuroendocrine cells of the pancreas. These types of cancer are called pancreatic neuroendocrine tumors, islet cell tumors or pancreatic endocrine cancer.
Factors that may increase your risk of pancreatic cancer include:
- Smoking
- Diabetes
- Chronic inflammation of the pancreas (pancreatitis)
- Family history of genetic syndromes that can increase cancer risk, Family history of pancreatic cancer
- Obesity
- Older age, as most people are diagnosed after age 65
Symptoms
Signs and symptoms of pancreatic cancer often don't occur until the disease is advanced. They may include:
- Abdominal pain that radiates to your back
- Loss of appetite or unintended weight loss
- Yellowing of your skin and the whites of your eyes (jaundice)
- Light-colored stools
- Dark-colored urine
- Itchy skin
- New diagnosis of diabetes or existing diabetes that's becoming more difficult to control
- Blood clots
- Fatigue
Treatment
In addition to a history and physical exam, imaging tests will be performed to help make the diagnosis of pancreatic cancer. These tests include:
- Ultrasound
- CT scanning
- MRI
- Endoscopic ultrasonography
- Endoscopic retrograde cholangiopancreatography (ERCP)
A definitive diagnosis of pancreatic cancer only comes from removal of tissue (biopsy) for examination in a lab. This can be done with a needle through the skin, during endoscopy, or with an operation.
Pancreatic cancer is treated in several ways, alone or in combination: Surgery
- Chemotherapy
- Immunotherapy
- Radiation therapy
- Targeted therapy
- Palliative care
Surgery is generally done to attempt to cure pancreatic cancer, but it may also be done to lessen or prevent symptoms. Chemotherapy and radiation are often given together, prior to, after, or even without surgery, to slow pancreatic cancer's growth. Targeted therapy is sometimes given to treat advanced pancreatic cancer. Immunotherapy can be given to people whose cancer cells have certain gene changes.Palliative care aims to reduce discomfort for people whose pancreatic cancer cannot be cured.
Preventive measures
You may reduce your risk of pancreatic cancer if you:
- Stop smoking
- Maintain a healthy weight
- Choose a healthy diet
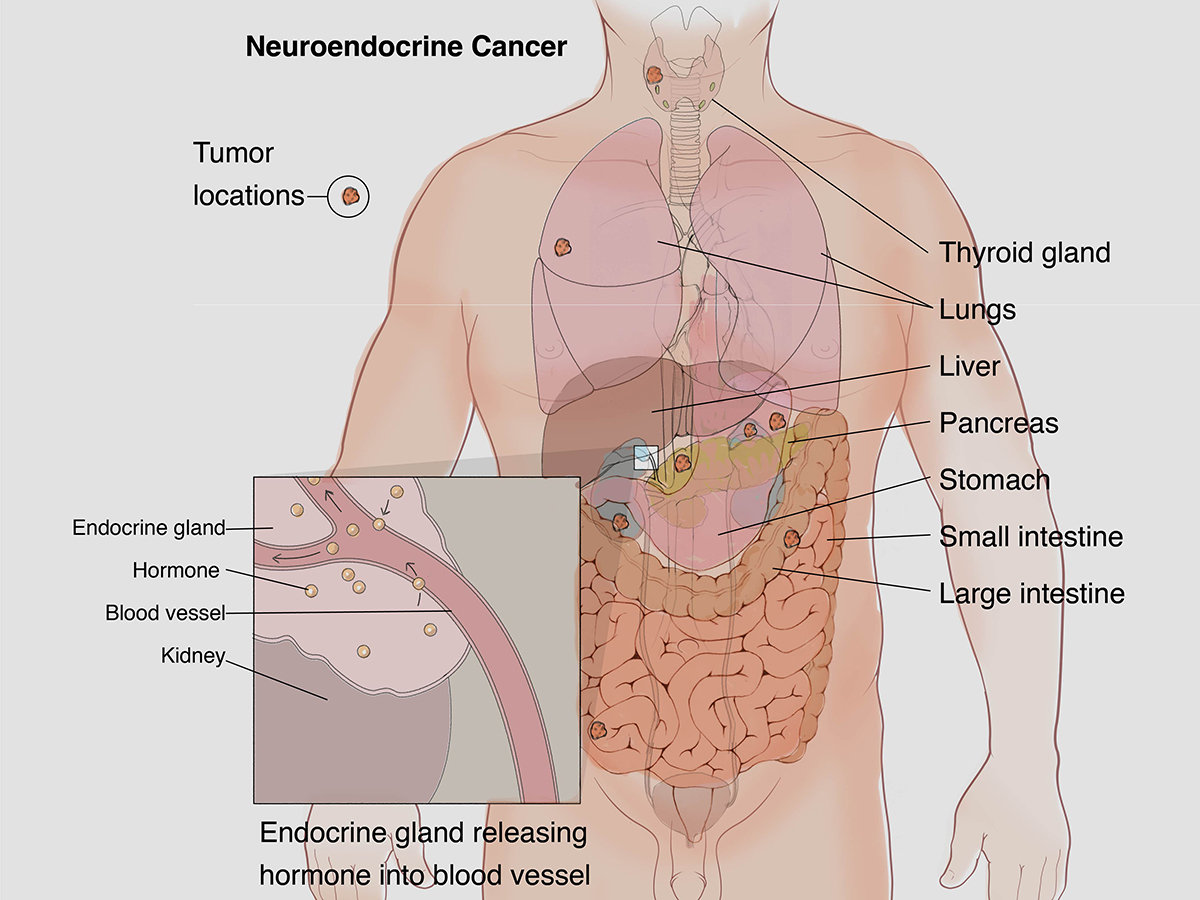
What is neuroendocrine tumors
Neuroendocrine tumors are cancers that begin in specialized cells called neuroendocrine cells. Neuroendocrine cells have traits similar to those of nerve cells and hormone-producing cells.
Neuroendocrine tumors are rare and can occur anywhere in the body. Most neuroendocrine tumors occur in the lungs, appendix, small intestine, rectum and pancreas.
There are many types of neuroendocrine tumors. Some grow slowly and some grow very quickly. Some neuroendocrine tumors produce excess hormones (functional neuroendocrine tumors). Others don't release hormones or don't release enough to cause symptoms (nonfunctional neuroendocrine tumors).
Causes
Most of the time, doctors don't know what causes NETs. But you're more likely to get them if you have certain diseases that run in your family, such as:
Multiple endocrine neoplasia type 1. This causes tumors to grow in the pancreas and other organs.
Neurofibromatosis type 1. This can cause tumors in your adrenal glands.
Von Hippel-Lindau syndrome. It makes tumors and fluid-filled sacs form in many parts of your body.
Symptoms
The symptoms you might experience depend on the location of your tumor and whether it produces excess hormones.
In general, neuroendocrine tumor signs and symptoms might include:
- Pain from a growing tumor
- A growing lump you can feel under the skin
- Feeling unusually tired
- Losing weight without trying
Neuroendocrine tumors that produce excess hormones (functional tumors) might cause:
- Skin flushing
- Diarrhea
- Frequent urination
- Increased thirst
- Dizziness
- Shakiness
- Skin rash
Treatment
In general, tests might include:
Aside from the urgent need to stop the bleeding, treatment is also aimed at preventing more bleeding. Procedures that help treat bleeding varices include:
- Physical exam
- Tests to look for excess hormones
- Imaging tests You might undergo imaging tests, such as ultrasound, CT and MRI, to create pictures of your tumor. For neuroendocrine tumors, pictures are sometimes created using positron emission tomography (PET) with a radioactive tracer that's injected into a vein.
- Procedures to remove a sample of cells for testing (biopsy) To collect the cells, a thin tube with a light and a camera on the end into your lungs (bronchoscopy), your esophagus (endoscopy) or your rectum (colonoscopy), depending on your situation. Sometimes, collecting a tissue sample requires surgery.
The treatment options for your neuroendocrine tumor will depend on the type of tumor, its location, and whether you're experiencing signs and symptoms of excess hormones produced by the tumor.
In general, neuroendocrine tumor treatment options might include:
- Surgery Surgery is used to remove the tumor. When possible, surgeons work to remove the entire tumor and some of the healthy tissue that surrounds it.
- Chemotherapy Chemotherapy uses strong drugs to kill tumor cells. It can be given through a vein in your arm or taken as a pill. Chemotherapy might be recommended if there's a risk that your neuroendocrine tumor might recur after surgery.
- Targeted drug therapy Targeted drug treatments focus on specific abnormalities present within tumor cells. By blocking these abnormalities, targeted drug treatments can cause tumor cells to die. Targeted drug therapy is usually combined with chemotherapy for advanced neuroendocrine tumors.
- Peptide receptor radionuclide therapy (PRRT) PRRT combines a drug that targets cancer cells with a small amount of a radioactive substance. It allows radiation to be delivered directly to the cancer cells. One PRRT drug, lutetium Lu 177 dotatate (Lutathera), is used to treat advanced neuroendocrine tumors.
- Medications to control excess hormones If your neuroendocrine tumor releases excess hormones, your doctor might recommend medications to control your signs and symptoms.
- Radiation therapy Radiation therapy uses powerful energy beams, such as X-rays and protons, to kill tumor cells. Some types of neuroendocrine tumors may respond to radiation therapy. It might be recommended if surgery isn't an option.