Hernia
Information you need to understand your disease and the tests you may need.
What is incisional hernia
An incisional hernia is the protrusion of abdominal tissue or parts of organs through the abdominal wall. They usually appear along, or close to, surgical scars on the abdomen.
Incisional hernia can develop weeks, months, or even years after abdominal surgery. People may notice a lump close to an abdominal scar, especially when coughing or straining the abdomen in any way. Most incisional hernias are not serious. However, they can get larger over time, which may affect normal breathing and movement. Large hernias can also be more challenging to operate on than smaller hernias. People may require surgery to repair an incisional hernia. If an incisional hernia is small, not causing any problems, and has a low chance of causing complications, people may not need surgery.

Causes
Incisional hernias happen when the surgical cut in your abdominal wall doesn’t close properly after surgery. This can cause your abdominal muscles to weaken, allowing tissue and organs to form a hernia.
Several things can prevent the surgical cut from healing properly, including:
- putting too much pressure on your abdomen
- becoming pregnant before the cut fully heals
- getting back into physical activities too soon after surgery
Several risk factors can increase the chances of a hernia developing after surgery, including:
- wound infection
- existing health conditions, such as renal failure, diabetes, or lung disease
- obesity
- smoking
- certain medications, including immunosuppressant drugs or steroids
Hernias are more likely after emergency surgery or surgery that requires a large incision. If the edges of the wound aren’t properly aligned after surgery, the incision may not heal well, increasing the likelihood of a hernia. The sewing technique used to close the incision can also play a part.
Symptoms
The most noticeable symptom of an incisional hernia is a bulge near the incision site. It’s often most visible when you strain your muscles, such as when you stand up, lift something, or cough.
Besides a visible bulge, incisional hernias might also cause:
- nausea and vomiting
- fever
- burning or aching near the hernia
- abdominal pain and discomfort, particularly around the hernia
- faster heartbeat than usual
- constipation
- diarrhea
- thin, narrow stool
Treatment
Hernias don’t go away on their own and are only treatable with surgery.
Small or reducible hernias
If you have a small or reducible hernia, you may be able to safely delay surgery. Your medical history and other factors will be considered when deciding if surgery will repair the hernia.If your hernia causes little or no discomfort, it may be safe to watch the hernia and wait before having surgery.
Large or irreducible hernias
If your hernia grows or becomes irreducible, you’ll need surgery. The recommended option will generally depend on your symptoms, the size of the hernia, and your medical history.
Open repair
Open hernia repair involves an incision at the hernia site.Your tissue, intestine, and other organs forming the hernia will be moved back into the abdomen and the opening will be closed.
Mesh patches might be used to reinforce the spot where the hernia developed. These mesh patches are sewn to the tissue around the hernia, where they’ll eventually be absorbed by your abdominal wall.
Laparoscopic repair
Laparoscopic hernia repair involves multiple small cuts instead of one large cut. Hollow tubes are placed in these incisions, and air inflates your abdomen to make your organs more visible. A surgical tool will be inserted, including a small camera, into the tubes to perform the surgery. Mesh may also be used in a laparoscopic repair.
Laparoscopic surgery is less invasive, and you may leave the hospital sooner and have a lower risk of infection.
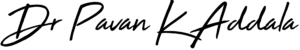
What is anal inguinal hernia
Inguinal hernia is when a piece of your intestine or part of the membrane lining your abdominal cavity -- the space that holds organs like your stomach, small intestines, liver, and kidneys -- pokes through a weak spot in your abdominal muscles near your groin. A physical exam is usually all it takes to diagnose the problem. If the hernia is large enough, you'll need surgery to fix it.
Causes
Some inguinal hernias have no apparent cause. Others might occur as a result of:
- Increased pressure within the abdomen
- A preexisting weak spot in the abdominal wall
- Straining during bowel movements or urination
- Strenuous activity
- Pregnancy
- Chronic coughing or sneezing
In many people, the abdominal wall weakness that leads to an inguinal hernia occurs prior to birth when a weakness in the abdominal wall muscle doesn't close properly. Other inguinal hernias develop later in life when muscles weaken or deteriorate due to aging, strenuous physical activity or coughing that accompanies smoking.
Weaknesses can also occur in the abdominal wall later in life, especially after an injury or abdominal surgery.
Symptoms
Inguinal hernia signs and symptoms include:
- A bulge in the area on either side of your pubic bone, which becomes more obvious when you're upright, especially if you cough or strain
- A burning or aching sensation at the bulge
- Pain or discomfort in your groin, especially when bending over, coughing or lifting
- A heavy or dragging sensation in your groin
- Weakness or pressure in your groin
- Occasionally, pain and swelling around the testicles when the protruding intestine descends into the scrotum
If you aren't able to push the hernia in, the contents of the hernia may be trapped (incarcerated) in the abdominal wall. An incarcerated hernia can become strangulated, which cuts off the blood flow to the tissue that's trapped. A strangulated hernia can be life-threatening if it isn't treated.
Signs and symptoms of a strangulated hernia include:
- nausea, vomiting or both
- Fever
- Sudden pain that quickly intensifies
- A hernia bulge that turns red, purple or dark
- Inability to move your bowels or pass gas
Treatment
A physical exam is usually all that's needed to diagnose an inguinal hernia to check a bulge in the groin area. Because standing and coughing can make a hernia more prominent, you'll likely be asked to stand and cough or strain.
If the diagnosis isn't readily apparent, imaging test, such as an abdominal ultrasound, CT scan or MRI might be recommended
If your hernia is small and isn't bothering you, watchful waiting will be suggested. Sometimes, wearing a supportive truss may help relieve symptoms, but check with your doctor first because it's important that the truss fits properly, and is being used appropriately.
Enlarging or painful hernias usually require surgery to relieve discomfort and prevent serious complications.
There are two general types of hernia operations — open hernia repair and minimally invasive hernia repair.
Open hernia repair
In this procedure, which might be done with local anesthesia and sedation or general anesthesia, an incision is made in your groin and the protruding tissue is pushed back into your abdomen. The weakened area is sewed, often reinforcing it with a synthetic mesh (hernioplasty). The opening is then closed with stitches, staples or surgical glue.
After the surgery, you'll be encouraged to move about as soon as possible, but it might be several weeks before you're able to resume normal activities.
Minimally invasive hernia repair
In this procedure requiring general anesthesia, the operation happens through several small incisions in your abdomen. Laparoscopic or robotic instruments will be used to repair your hernia. Gas is used to inflate your abdomen to make the internal organs easier to see.
A small tube equipped with a tiny camera (laparoscope) is inserted into one incision. Guided by the camera, tiny instruments are inserted through other small incisions to repair the hernia using synthetic mesh.
People who have a minimally invasive repair might have less discomfort and scarring after surgery and a quicker return to normal activities. Long-term results of laparoscopic and open hernia surgeries are comparable.
Minimally invasive hernia surgery helps to avoid scar tissue from an earlier hernia repair, so it might be a good choice for people whose hernias recur after open hernia surgery. It also might be a good choice for people with hernias on both sides of the body (bilateral). As with open surgery, it may be a few weeks before you can get back to your usual activity level.
Preventive measures
You can't prevent the congenital defect that makes you susceptible to an inguinal hernia. You can, however, reduce strain on your abdominal muscles and tissues.
For example:
- Maintain a healthy weight.
- Emphasize high-fiber foods.
- Lift heavy objects carefully or avoid heavy lifting.
- Stop smoking.
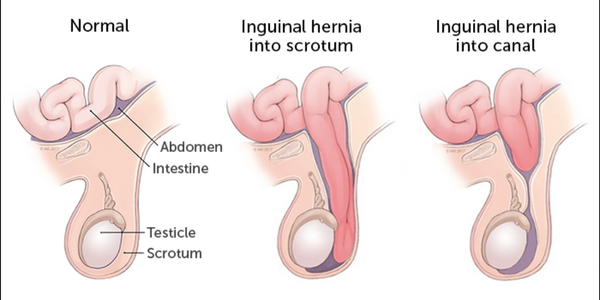
What is anal umbilical hernia
An umbilical hernia occurs when part of your intestine bulges through the opening in your abdominal muscles near your belly button (navel). Umbilical hernias are common and typically harmless.
Umbilical hernias are most common in infants, but they can affect adults as well. Children's umbilical hernias often close on their own in the first two years of life, though some remain open into the fifth year or longer. Umbilical hernias that appear during adulthood are more likely to need surgical repair.
Causes
During gestation, the umbilical cord passes through a small opening in the baby's abdominal muscles. The opening normally closes just after birth. If the muscles don't join together completely in the midline of the abdominal wall, an umbilical hernia may appear at birth or later in life.
In adults, too much abdominal pressure contributes to umbilical hernias. Causes of increased pressure in the abdomen include:
- Obesity
- Multiple pregnancies
- Fluid in the abdominal cavity
- Previous abdominal surgery
- Long-term peritoneal dialysis to treat kidney failure
Symptoms
An umbilical hernia creates a soft swelling or bulge near the navel. In babies who have an umbilical hernia, the bulge may be visible only when they cry, cough or strain. Umbilical hernias in children are usually painless. Umbilical hernias that appear during adulthood may cause abdominal discomfort.
Seek emergency care if your baby has an umbilical hernia and:
- Appears to be in pain
- Begins to vomit
- Has tenderness, swelling or discoloration at the site of the hernia
Similar guidelines apply to adults. Seek emergency care if the bulge becomes painful or tender. Prompt diagnosis and treatment can help prevent complications. Adults with umbilical hernias are somewhat more likely to experience a blockage of the intestines. Emergency surgery is typically required to treat these complications.
Treatment
An umbilical hernia is diagnosed during a physical exam. Sometimes imaging studies — such as an abdominal ultrasound or a CT scan — are used to screen for complications.
For children, surgery is typically reserved for umbilical hernias that:
- Are painful
- Are slightly larger than 1/4 to 3/4 inch (1 to 2 centimeters) in diameter
- Are large and don't decrease in size over the first two years of life
- Don't disappear by age 5
- Become trapped or block the intestine
For adults, surgery is typically recommended to avoid possible complications, especially if the umbilical hernia gets bigger or becomes painful.
During surgery, a small incision is made near the bellybutton. The herniated tissue is returned to the abdominal cavity, and the opening in the abdominal wall is stitched closed. In adults, mesh is often used to help strengthen the abdominal wall.
If you have surgery to repair your umbilical hernia, your recovery time will depend on its size and how difficult your surgery was. Both children and adults who have surgery typically go home the same day of the procedure. Usually you’ll need about 3 to 5 days to rest and heal. You shouldn’t lift anything heavy for about 3 weeks after surgery. Once your umbilical hernia goes away, either on its own or with surgery, it’s not likely it will come back.
What is femoral hernia
A femoral hernia will appear as a bulge near the groin or thigh. your intra-abdominal tissues can be pushed through a weakened spot in your muscle when you overstrain. If a portion of tissue pushes through the wall of the femoral canal, it’s called a femoral hernia. Most femoral hernias do not cause symptoms. However, they can occasionally lead to severe problems if the hernia obstructs and blocks blood flow to your intestines. This is called a strangulated hernia — it’s a medical emergency and requires immediate surgery.

Causes
You may be born with a weakened area of the femoral canal, or the area may become weak over time.Straining can contribute to the weakening of the muscle walls. Factors that can lead to overstraining include:
Causes of esophageal varices include:
- Childbirth
- chronic constipation
- heavy lifting
- being overweight
- difficult urination due to an enlarged prostate
- chronic coughing
Symptoms
Small and moderate-sized hernias don’t usually cause any symptoms. In many cases, you may not even see the bulge of a small femoral hernia. Large hernias may be more noticeable and can cause some discomfort. A bulge may be visible in the groin area near your upper thigh. The bulging may become worse and can cause pain when you stand up, lift heavy objects, or strain in any way. Femoral hernias are often located very close to the hip bone and as a result may cause hip pain. Severe symptoms of a femoral hernia include:
- severe stomach pain
- sudden groin pain
- Nausea
- vomiting
Treatment
A physical examination will be performed by gently palpating, or touching, the area to determine if you have a femoral hernia. If the hernia is large, the bulging will most likely be felt. Ultrasound of the abdominal and groin area can confirm the diagnosis or establish a diagnosis if suspicion of a femoral hernia is high but no bulge is evident on physical examination. Imaging technology can show the defect in the muscle wall, as well as the protruding tissue.
Moderate to large femoral hernias require surgical repair, especially if they’re causing any level of discomfort.Surgical hernia repair is performed under general anesthesia. Femoral hernia repair can be done as either an open or laparoscopic surgery. An open procedure requires a larger incision and a longer recovery period. Laparoscopic surgery uses three to four keyhole-sized incisions that minimize loss of blood. Laparoscopic surgery, for instance, involves less pain and scarring than open surgery, as well as a shorter time required for healing.
In both surgeries, incisions will be made in your groin area to access the hernia. The intestine or other tissue protruding from the femoral area is returned to its proper position. The hole will be sewed back together and may be reinforced with a piece of mesh. The mesh strengthens the wall of the canal.
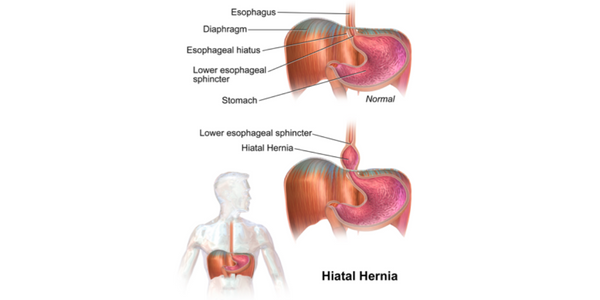
What is hiatal hernia
A hiatal hernia occurs when the upper part of your stomach bulges through the large muscle separating your abdomen and chest (diaphragm). Your diaphragm has a small opening (hiatus) through which your food tube (esophagus) passes before connecting to your stomach.
In a hiatal hernia, the stomach pushes up through that opening and into your chest. A large hiatal hernia can allow food and acid to back up into your esophagus, leading to heartburn.
Causes
Causes might include:
- Being born with a larger hiatal opening than usual
- Injury to the area
- Changes in your diaphragm as you age
- A rise in pressure in your belly, as from pregnancy, obesity, coughing, lifting something heavy, or straining on the toilet
Symptoms
Many people with hiatal hernia don’t notice any symptoms. Others may have.
- Heartburn from gastroesophageal reflux disease (GERD)
- Chest pain
- Bloating
- Burping
- Trouble swallowing
- Bad taste in your mouth
- An upset stomach and vomiting
- Backflow of food or liquid from your stomach into your mouth
- Shortness of breath
Treatment
To diagnose a hiatal hernia, following tests might be necessary
- Barium swallow. You drink a liquid that shows up on an X-ray so a better look at your esophagus and stomach can be taken
- Endoscopy..
- Esophageal manometry (pressure study). A different kind of tube goes down your throat to check the pressure in your esophagus when you swallow.
- pH test. This measures the acid levels in your esophagus.
If you have acid reflux, medications may be suggested to treat those symptoms, including:
- Antacids to weaken your stomach acid
- Proton pump inhibitors or H-2 receptor blockers to keep your stomach from making as much acid
- Prokinetics to make your esophageal sphincter -- the muscle that keeps stomach acid from backing up into your esophagus -- stronger.
Surgery might be required if you have a paraesophageal hernia (when part of your stomach squeezes through the hiatus) so your stomach doesn’t become strangled. You may also need surgery if sliding hernias bleed or become large, strangulated, or inflamed.In surgery, your hiatus will be reinforced and move your stomach. Many hiatal hernia surgeries use a method called laparoscopy. They insert a tool called a laparoscope through incisions, and it sends pictures to a monitor. These “minimally invasive” procedures have smaller cuts, less risk of infection, less pain and scarring, and faster recovery than traditional surgeries. You can probably go back to regular activity in 2 weeks
Preventive measures
Some changes to your daily life can help with acid reflux symptoms. They include:
- Don’t exercise or lie down for 3 or 4 hours after you eat.
- Avoid acidic foods like orange juice, tomato sauce, and soda.
- A diet of mashed and soft foods is recommended for up to 2-3 weeks after surgery.
- Limit fried and fatty foods, alcohol, vinegar, chocolate, and caffeine.
- Eat smaller meals (four or five small meals each day) and eat slowly.
- Lift the head of your bed about 6 inches.
- Don’t wear tight belts or clothes that put pressure on your belly.
- Lose extra pounds.
- Don’t smoke. Smoking is an intense heartburn generator.
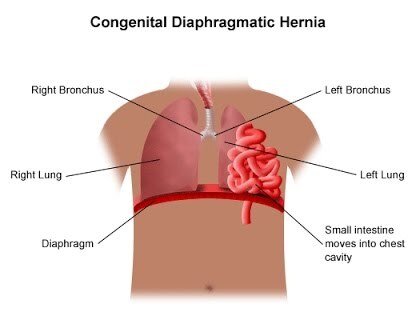
What is diaphragmatic hernia
The diaphragm is a dome-shaped muscular barrier between the chest and abdominal cavities. It separates your heart and lungs from your abdominal organs (stomach, intestines, spleen, and liver). A diaphragmatic hernia occurs when one or more of your abdominal organs move upward into your chest through a defect (opening) in the diaphragm. This kind of defect can be present at birth or acquired later in life.
Causes
A congenital diaphragmatic hernia (CDH) is due to the abnormal development of the diaphragm while the fetus is forming. A defect in the diaphragm of the fetus allows one or more of their abdominal organs to move into the chest and occupy the space where their lungs should be. As a result, the lungs can’t develop properly.An acquired diaphragmatic hernia (ADH) is usually the result of a blunt or penetrating injury. Traffic accidents and falls cause the majority of blunt injuries. Penetrating injuries are usually due to stab or gunshot wounds. Surgery on the abdomen or chest may also cause accidental damage to your diaphragm. Rarely, the diaphragmatic hernia may occur without a known reason and go undiagnosed for a period of time, until it becomes severe enough to cause symptoms.
Symptoms
The severity of symptoms with a diaphragmatic hernia can vary depending on its size, cause, and the organs involved.
- Difficulty breathing: This is usually very severe. In a CDH, it results from the abnormal development of the lungs. In an ADH, it occurs when the lungs can’t function properly due to crowding.
- Tachypnea (rapid breathing): Your lungs may try to compensate for the low levels of oxygen in your body by working at a faster rate.
- Blue discoloration of the skin: When your body doesn’t receive enough oxygen from your lungs, it can make your skin appear blue (cyanosis).
- Tachycardia (rapid heart rate): Your heart may pump more rapidly than normal to try to supply your body with oxygenated blood.
- Diminished or absent breath sounds: This symptom is common in the case of a CDH because one of the baby’s lungs may not have formed properly.
- Bowel sounds in the chest area: This occurs when your intestines move up into your chest cavity.
- Less full abdomen: Your abdomen may be less full than it should upon palpation (an examination of the body by pressing on certain areas). This is due to abdominal organs being pushed up into the chest cavity.
Treatment
The following tests are usually sufficient to diagnose either a CDH or an ADH:
- X-ray
- ultrasound scan
- CT scan
- arterial blood gas test (takes blood directly from an artery and tests for levels of oxygen, carbon dioxide, and acidity, or pH level)
- MRI
Both congenital and acquired diaphragmatic hernias typically require urgent surgery. Surgery must be performed to remove the abdominal organs from the chest and place them back into the abdomen. The diaphragm will be repaired then.
With a CDH, we may perform surgery as early as 48 to 72 hours after the baby is delivered. The first step is to stabilize the baby and increase its oxygen levels. A variety of medications and techniques are used to help stabilize the infant and assist with breathing. These babies are best cared for at a center with a highly specialized Neonatal Intensive Care Unit (NICU). Once the baby stabilizes, then surgery can occur.
With an ADH, the patient typically needs to be stabilized before surgery. Because most cases of ADH are due to injury, there might be other complications such as internal bleeding. Therefore, the surgery should happen as soon as possible.
Preventive measures
Currently, there is no known way to prevent a CDH. Early and regular prenatal care during pregnancy is important to help detect the problem before birth. This allows for proper planning and care before, during, and after delivery.
Some basic preventive measures that can help you avoid an ADH include:
- Driving safely and always wearing a seat belt.
- Avoiding activities that make you prone to significant blunt injuries to the chest or abdomen, such as extreme sports.
- Limiting alcohol and avoiding drug use which can make you more prone to accidents.
- Exercising caution around sharp objects, such as knives and scissors.